A sleep issue that afflicts over a third of Americans, up to 70 million people, has been shown to drastically raise the risk of developing multiple health conditions, including obesity, heart disease and dementia.
While a landmark Mayo Clinic study recently highlighted a 40 per cent increased risk of dementia, equivalent to 3.5 years of accelerated brain aging, the detrimental impact of insomnia extends far beyond neurology.
Insomnia is a key contributor to the development and worsening of high blood pressure, heart disease, stroke, obesity and type 2 diabetes, while also crippling the immune system and leaving people more vulnerable to infections.
The core symptoms of insomnia include difficulty and delay in falling asleep, difficulty staying asleep, waking up too early or being unable to fall back to sleep.
Widespread harm occurs because sleep is a vital biological requirement for maintenance and repair. When the cycle of chronic insomnia prevents essential restoration, it triggers a cascade of hormonal imbalances, rampant inflammation and accumulated cell damage.
This domino effect strains the cardiovascular system, disrupts metabolic function and compromises the body’s fundamental defenses, positioning chronic insomnia as a critical yet modifiable risk factor for some of the most devastating diseases in the US.
Sleep is also crucial for overall brain health. Drifting off at night initiates a cleaning process to discard waste and toxins the brain has accumulated while awake.
The brain cannot complete this core process during wakefulness, which allows toxins like inflammatory markers and proteins linked to Alzheimer’s and other dementias to accumulate, potentially leading to atrophy in parts of the brain that govern memory, executive functioning, and movement.

Up to 70 million Americans live with insomnia, which involves difficulty and delay in falling asleep, difficulty staying asleep and waking up too early in the morning or being unable to fall back to sleep
Dementia
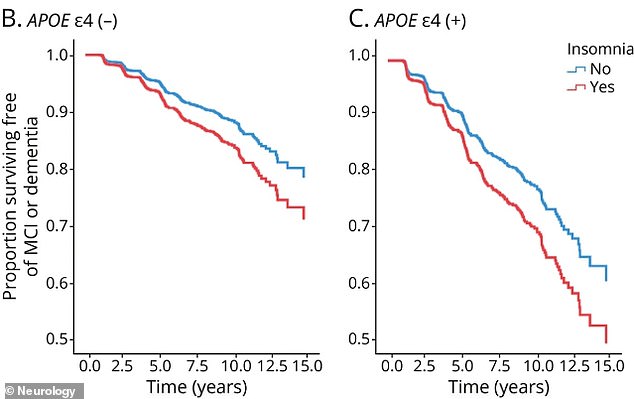
Chronic insomnia increased the risk of cognitive impairment by 40 per cent. While this risk applies to everyone, it was more pronounced in those without the APOE4 gene (Panel B). For carriers (Panel C), the overwhelming risk from their genetics is so high that the additional impact of insomnia is less noticeable
A long-term study of adults aged 50 and older, with an average age of 70, has linked chronic insomnia to accelerated cognitive decline and an increased risk of dementia.
The research, analyzing data from the Mayo Clinic Study of Aging, found that individuals with chronic insomnia were 40 per cent more likely to develop mild cognitive impairment or dementia.
Their brains also exhibited signs of accelerated aging, comparable to being nearly four years older.
The study associated insomnia with tangible biological damage, including a greater accumulation of Alzheimer’s-related proteins.
Insufficient sleep is known to impede the clearance of amyloid-beta, leading to plaque buildup, and can increase levels of tau, a protein that forms toxic tangles.
For carriers of the APOE4 gene, a known genetic risk factor for Alzheimer’s, chronic insomnia led to even steeper declines in cognitive function. Roughly 20 to 25 percent of Americans carry one copy of this gene, while two percent carry two.
These findings suggest that chronic insomnia may act as both an early warning sign and a potential contributor to future cognitive impairment, underscoring its significant impact on long-term brain health.
It was published in the journal Neurology.
Heart disease
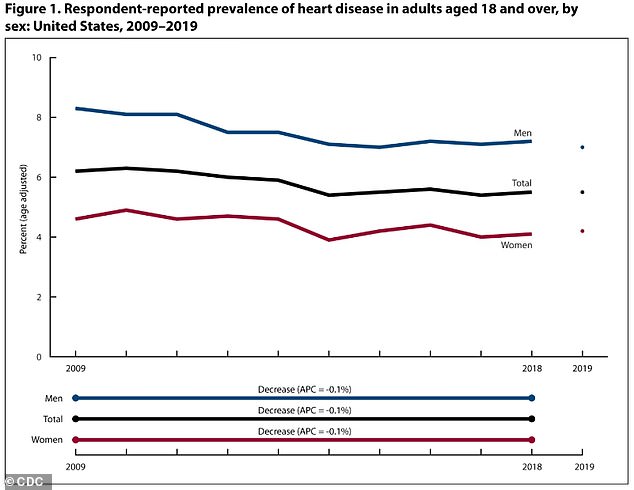
Age-adjusted heart disease rates fell from 2009 to 2019 but remained higher in men (8.3 percent to 7.0 percent) than in women (4.6 percent to 4.2 percent)
When the body is consistently deprived of adequate sleep, it enters a state of heightened stress.
The body overproduces cortisol, a hormone that, in chronic excess, keeps the body in a constant ‘fight-or-flight’ mode, which raises heart rate and blood pressure, putting undue strain on the heart.
Sleep is also crucial for regulating the immune system. Without it, the body produces an excess of inflammatory cytokines, proteins that play a role in immune response. This creates a state of persistent, low-grade inflammation throughout the cardiovascular system.
Together, high cortisol and chronic inflammation damage the smooth, protective lining of blood vessels. which is the primary driver of atherosclerosis, a process where plaque, made of fat, cholesterol, and other substances, builds up inside the arteries, hardening and narrowing them.
Hardened, narrowed arteries greatly increase the risk of heart attack, stroke, and other cardiovascular diseases.
An estimated 121.5 million American adults, nearly 49 percent, have some form of heart disease, including coronary artery disease, heart failure, and stroke
High blood pressure
A key function of sleep is to give the cardiovascular system rest.
In a well-regulated body, blood pressure follows the body’s sleep-wake rhythm, dipping significantly during the night. The dip allows the heart to work less vigorously and the walls of blood vessels and arteries to relax.
When sleep is disrupted or cut short, this vital dip does not occur. As a result, the heart and blood vessels are forced to operate at daytime pressure levels for 24 hours a day, placing them under non-stop stress.
The constant pressure is a major contributor to the long-term development of hypertension, or high blood pressure, and cardiovascular disease.
Around 115 million adults, nearly half of the population, has high blood pressure.
Weight gain and obesity
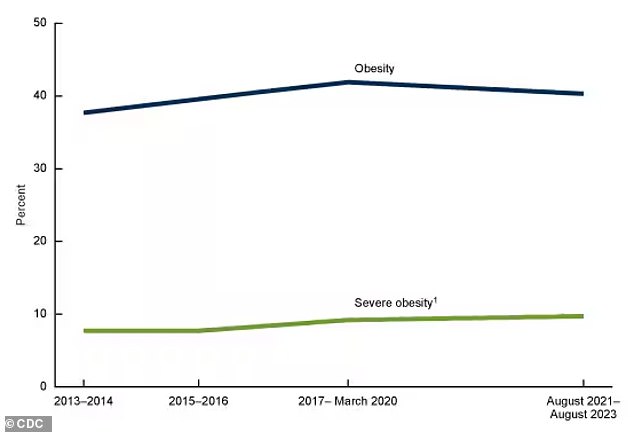
The above graph shows findings from a new CDC report, reflecting the most recent available data, which shows that obesity rates have fallen slightly for the first time ever, though they still remain higher than 2013-2014
Insomnia and sleep deprivation disrupt key hormones that regulate appetite, including an increase in ghrelin, the hormone that stimulates hunger, and a decrease in leptin, the hormone that signals satiety.
The resulting hormonal imbalance directly leads to increased feelings of hunger and a reduced sense of fullness.
Beyond this shift, sleep loss also affects neurological reward pathways. It amplifies the perceived pleasure and reward value of high-calorie, carbohydrate-dense, and fatty foods, influencing poorer dietary choices.
Insufficient sleep is also interpreted by the body as a stressor, elevating levels of the stress hormone cortisol.
This stress response further promotes cravings for comfort foods, which are often energy-dense or ultra-processed, creating a compounded effect that significantly increases the likelihood of overeating.
Approximately 40 percent of American adults have obesity, equating to around 100 million individuals. That number has steadily risen in recent decades as food has become more and more processed and Americans have become more sedentary.
Type 2 Diabetes
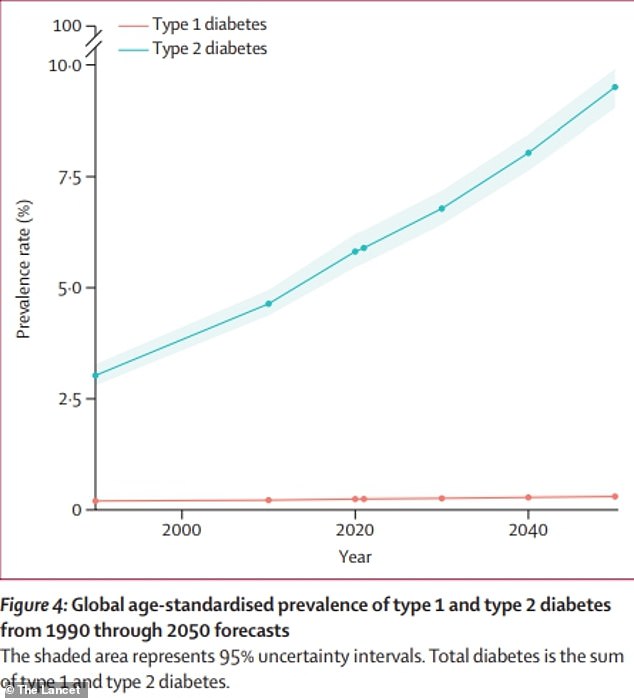
The above graph shows estimates for global diabetes cases. It is predicted that the number of people with the condition will more than double by the year 2050 compared to 2021
Insufficient or poor-quality sleep hinders the body’s ability to regulate blood sugar, promoting the development of insulin resistance, a primary risk factor for type 2 diabetes.
Sleep deprivation reduces the body’s sensitivity to insulin, the hormone essential for transporting glucose from the bloodstream into cells for energy.
To compensate for this reduced sensitivity, the pancreas must produce greater amounts of insulin to maintain normal blood sugar levels. This increased demand places strain on the pancreas over time.
Poor sleep can elevate inflammation throughout the body. Both weight gain and inflammation are established factors that worsen insulin resistance, which then creates a harmful cycle that significantly elevates the risk for developing type 2 diabetes and other metabolic disorders.
As of 2021, an estimated 38.4 million Americans had diabetes, with approximately 90 to 95 percent of them having type 2 diabetes, translating to about 1 in 10 Americans.
Infections
Chronic insomnia compromises immune function, elevating a person’s risk of contracting common infectious germs such as cold and influenza viruses.
Sleep provides a critical period for the immune system to regulate itself, during which time the body produces essential proteins like cytokines and aids in the generation of immune cells.
Insufficient sleep can reduce the production and efficacy of key immune cells, including T-cells and white blood cells, which are necessary for identifying and eliminating harmful invaders.
Sleep deprivation also disrupts the release of cytokines during the sleep-wake cycle, proteins that are vital for coordinating immune responses and managing inflammation.
A weakened defensive response and a potential increase in pro-inflammatory cytokines creates a state of chronic, low-grade inflammation that undermines the integrity of the immune system, which mounts a less effective response to challenges.
This can be seen in a reduced antibody production following vaccination and a prolonged recovery time from illness.











