A common food poisoning bug that spreads through contaminated food and water could be fueling the colon cancer epidemic in young people, a study suggests.
Colorectal cancer, long considered a disease of old age, is increasingly striking people in their 20s, 30s and 40s in the US and UK in a phenomenon that has baffled doctors.
Researchers in Japan studying patients with Familial Adenomatous Polyposis (FAP), a genetic condition causing colon polyps, found that those harboring the toxic bacterium colibactin-producing E. coli (pks+) in their polyps were over three times more likely to have developed colorectal cancer.
Colibactin is a potent toxin that causes DNA damage, accelerating cancer development in people already highly vulnerable to colorectal cancer.
A person with FAP is born with a gene mutation that removes the brakes on cell division in the colon. This causes cells to multiply uncontrollably, clumping together to form hundreds of polyps and creating a genetically vulnerable landscape for cancer.
In their analysis of 75 patients with colon polyps due to FAP, they found that polyps containing the bacteria had more DNA damage and more inflammation, raising the risk of cancer, compared to the surrounding cells.
Colorectal cancer is the second most common cause of cancer death overall, after lung cancer. More than 154,000 Americans will be diagnosed with CRC this year, and an estimated 53,000 are projected to die.
While the study focused on people with a genetic disorder, it identified a toxic bacterium that can affect anyone. One in five healthy people without cancer harbors the bacteria in their gut. Meanwhile, the toxic bacterium was found in two-thirds of patients with colorectal cancer with no known hereditary cause.

CrossFit enthusiast Chris Rodriguez was diagnosed with cancer at 35 years old, despite also eating clean foods high in protein and fiber
Preventive surgery to remove the colon is considered the only definitive way to prevent colorectal cancer in patients with FAP.
Japanese researchers recruited 75 FAP patients who still had their colons.
During routine colonoscopies, researchers took small tissue samples from patients’ colon polyps.
Colon polyps are small, non-cancerous growths that develop on the lining of the colon. Some types, though, have a higher risk of developing into colon cancer.
The development of a cancerous polyp can take years, resulting from long-term, repeated environmental exposures and lifestyle factors that lead to the accumulation of genetic mutations and changes.
Those gene alterations work in concert with someone’s genes since birth that influence their susceptibility to developing cancer, to turn off the body’s control over cell death and replication, damaging DNA and causing cancer cells to grow and flourish.
The researchers analyzed the samples to find a toxic strain of E. coli bacteria that produces a DNA-damaging colibactin, known as pks+ E. coli.

TikTok star Bailey Hutchins has died at the age of 26 after a two-year battle with colon cancer

She was diagnosed with stage 4 colorectal cancer with peritoneal metastasis in 2023 at the age of 24
They then looked at the patients’ medical records to see who had already had colon cancer in their lives, planning to investigate why some FAP patients were previously diagnosed or had active cancer.
For FAP patients who had a history of colon cancer and who still had their colons, those with the toxic pks+ E. coli bacteria in their polyps were over three times more likely to have a history of colorectal cancer.
Polyps with the bacteria also showed significantly higher levels of a marker called γ-H2AX, indicating that the cells’ DNA was severely damaged. They also showed signs of inflammation, which creates an environment that fuels cancer growth.
When the researchers looked at the samples under a microscope, they saw that the polyps with the bacteria looked more abnormal and aggressive, with more immune cells infiltrating them, indicating the body was attempting to fight the damage.
The study, published in the journal eGastroenterology, found that FAP patients who had already gotten cancer were much more likely to have this harmful bacteria in their systems, suggesting that the bacteria plays a direct role in causing cancer to develop.
FAP is a rare genetic disorder, affecting an estimated one in 5,000 to 10,000 people in the US.
It is responsible for fewer than one percent of all colorectal cancer cases, which are ticking up in people in their 20s, 30s, 40s, and early 50s.
A study published earlier this month by the American Cancer Society reported that, after a stable 15-year trend, diagnoses of local-stage colorectal cancer (CRC) rose dramatically in American adults aged 45 to 49 years old between 2019 and 2022.
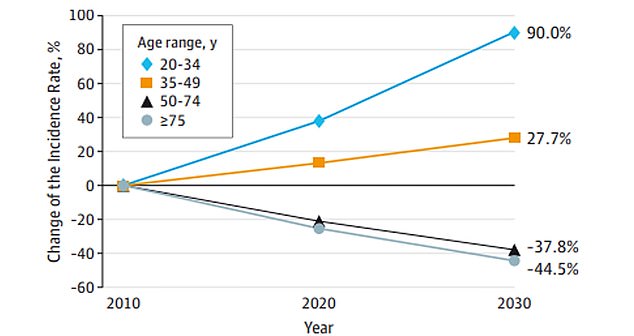
Data from JAMA Surgery showed colon cancer is expected to rise by 90 percent in people ages 20 to 34 by 2030
Among this age group, cases increased by one percent annually from 2004 to 2019, and then accelerated to 12 percent per year from 2019 to 2022.
In people aged 20 to 39 years old, CRC incidence has increased steadily by 1.6 percent annually since 2004.
Among adults aged 40 to 44 and 50 to 54 years old, the increase was 2 percent and 2.6 percent annually, respectively, since 2012.
Overall, from 2021 to 2022, there was a 50 percent relative increase in diagnoses, rising from 11.7 cases per 100,000 people to 17.5 cases per 100,000 people.
The ongoing surge has been driven by the detection of early, local-stage tumors, which increased from 2019 to 2022 by 19 percent per year for colon cancer and by 25 percent per year for rectal cancer.
Experts are still investigating the drivers of the trend, but have zeroed in on lifelong and society-wide changes in people’s gut microbiomes, an increasingly fatty diet made up of processed foods containing carcinogenic chemicals, low fiber intake, and record-high rates of obesity, a risk factor for cancer.











