Addiction warnings are being strengthened on some of the UK’s most widely prescribed pain, anxiety and sleep medicines.
The Medicines and Healthcare products Regulatory Agency (MHRA) ordered the move after a safety review flagged risks linked to gabapentinoid painkillers, benzodiazepine tranquillisers and Z-drugs used for sleep.
Patient information leaflets – covering treatments for conditions ranging from nerve pain to sleep disorders – will now carry the warning: ‘May cause addiction, dependence and withdrawal reactions’.
They will also spell out what addiction and dependence mean, offer clearer advice on tapering and stopping treatment safely, and urge patients to speak to healthcare professionals about risks.
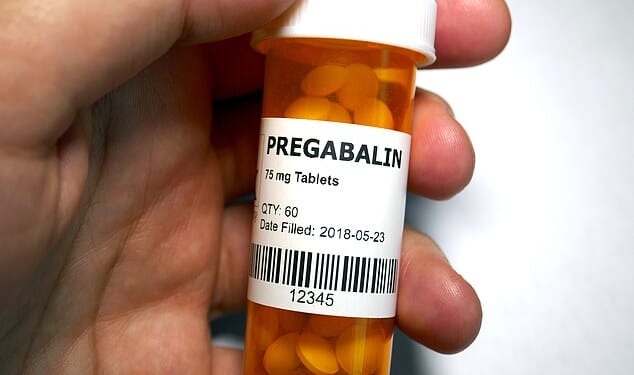
Gabapentinoids include drugs such as gabapentin and pregabalin, primarily prescribed for nerve pain and epilepsy but also used for conditions including anxiety.
NHS figures show that around 4.5 million people in England are prescribed one each year.
The drugs act on GABA pathways in the brain to relieve pain and produce sedative effects, but long-term use can lead to physical dependence and difficult withdrawal for some patients.
Addiction clinics report patients turning to online sellers or street dealers after building tolerance and needing higher doses to feel the effects.

Pregabalin is being given stronger addiction warnings
As part of the review, the Commission on Human Medicines (CHM) backed changes not only to packaging and patient information leaflets, but also stronger warnings not to combine the medicines with opioids or alcohol, and not to share them with others.
Benzodiazepines – a class of drugs used to treat severe anxiety or insomnia during acute crises – are typically prescribed only short term, with GPs usually issuing courses of two to four weeks.
Often referred to as ‘benzos’, those available on the NHS include diazepam – the most commonly used benzodiazepine in the UK – which is also prescribed to manage alcohol withdrawal. Others include lorazepam and temazepam, which are sometimes used before surgical procedures, and chlordiazepoxide, another drug used in alcohol withdrawal.
Clobazam and clonazepam are also benzodiazepines, but are primarily prescribed to treat epilepsy and seizures rather than anxiety.
Alprazolam – better known as Xanax – is not routinely prescribed on the NHS and is only available via private prescription in the UK.
Z-drugs are a separate class of non-benzodiazepine medicines used for the short-term treatment of severe insomnia. Despite the nickname ‘sleeping pills’, the ‘Z’ does not refer to sleep itself, but to the fact that many of the original drugs in the class begin with the letter Z.
The Z-drugs currently prescribed on the NHS are zopiclone – also known as Zimovane or Imovane – and zolpidem, sold under brand names including Ambien and Stilnoct. Another drug, zaleplon (Sonata or Starnoc), stopped being prescribed in the UK in 2004.
Dr Alison Cave, the MHRA’s chief safety officer, said: ‘Addiction and dependency can happen to anyone taking these medicines, even when used as directed.
‘That’s why we are strengthening warnings so patients and healthcare professionals can better understand the risks.
‘These medicines remain valuable treatments for many patients and it’s important they have the information they need to be able to use them safely.
‘If you have any questions about your medication use or side effects, please speak to a healthcare professional.
‘Do not stop taking your medicine without advice, as this could cause withdrawal symptoms.’