THE tragic deaths of Jennifer Cahill and her newborn daughter have laid bare serious failings that could cost more mothers and babies their lives, a coroner has warned.
The 34-year-old mum had chosen to deliver Agnes Lily at home after feeling “unsupported” in hospital following the birth of her first child.
But the delivery, which took place at their home in Manchester on June 3, 2024, descended into “chaos” when Agnes was born not breathing with the umbilical cord around her neck.
Jennifer – who, her husband Rob said, was never able to hold her baby – suffered a perineal tear, two postpartum haemorrhages, and later went into cardiac arrest.
She died the following day on June 4, while Agnes died in hospital four days later.
Jennifer‘s cause of death was determined as multi-organ failure due to cardiac arrest due to postpartum haemorrhage.
Agnes died from multi-organ failure, following hypoxia after umbilical cord compression.
On October 26, 2025, following a two-week inquest, senior coroner Joanne Kearsley concluded the family suffered a “Victorian-aged tragedy” played out in the modern day.
She determined that both deaths were contributed to by “neglect”, “catastrophic error” and “gross failures to provide basic care“.
Following the inquest, the coroner issued a Prevention of Future Deaths report, warning that more women and babies could die unless urgent action is taken.
“In my opinion there is a risk that future deaths will occur unless action is taken,” she wrote in the report published in November last year.
Central to the findings was the lack of any national, evidence-based guidance governing home births, leading to wide variation in practice across England.
“There is no national guidance to support consistent practice across the country including, for example, details of clinical scenarios where women, following robust assessment, have been considered too high risk to safely receive care in a home-setting,” the coroner wrote.
The report also warned that risks of death are not routinely discussed with women considering home births.
“Even though there is a very small risk of death, this is not something which is discussed with women particularly in relation to maternal death,” it said.
It added: “There is no guidance to ensure the risk of death to both mother and baby is discussed with any woman considering a home birth irrespective of being considered high or low risk.”
National Institute of Health and Care Excellence (NICE) only refers to the potential risk of death to a baby.
There is no mention in the guidance of risk to the mother.
The coroner refers to the confusion Jennifer faced, being told by doctors she was a low-risk pregnancy.
But it was not explained that she would have a high-risk delivery after previously suffering a postpartum haemorrhage with her first child three years earlier.
The court was told Jennifer chose a home birth for her second child after carrying out extensive research – believing the risk of bleeding was lower.
The inquest heard how, without understanding the distinction between the risk during pregnancy and delivery, Jennifer could not have made an informed decision about where to have her child.
Home deliveries pose a heightened danger to an already high-risk delivery.
The coroner also highlighted gaps in midwife training and experience, the absence of national data on emergency hospital transfers, and failures in basic monitoring during Jennifer’s labour.
Both deaths were found to have been contributed to by neglect, and the coroner ruled they would not have happened when they did if proper care had been provided.
What is postpartum haemorrhage?
Postpartum haemorrhage (PPH) is a complication where you bleed heavily from the vagina after your baby’s birth.
It is normal to bleed from your vagina after you have a baby.
Bleeding is usually heaviest just after birth and gradually becomes less over the next few hours.
The bleeding will reduce further over the next few days.
There are two types of PPH, depending on when the bleeding takes place:
- Primary or immediate – bleeding that happens within 24 hours of birth
- Secondary or delayed – bleeding that happens after the first 24 hours and up to 12 weeks after the birth
Sometimes PPH happens because your womb doesn’t contract strongly enough after the birth.
It can also happen because part of the placenta has been left in your womb or you get an infection in the lining of the womb
If heavy bleeding does occur, it is important that it is treated very quickly so that a minor haemorrhage doesn’t become a major haemorrhage, which can be life-threatening.
Sources: NHS, RCOG
‘We are committed to learning from incidents’
Manchester University NHS Foundation Trust accepted Jennifer should have been referred to a senior midwife after deciding on a home birth so the dangers could be discussed.
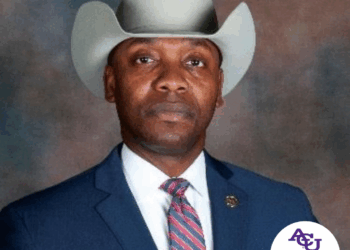
Kimberley Salmon-Jamieson, Deputy Chief Executive & Chief Nursing Officer, said: “I would like to once again offer our deepest condolences to the family and friends of Mrs Cahill and Agnes.
“We have been in regular contact with Mr Cahill following this tragic incident, including sharing the findings of both the internal and external safety investigations.
“The Trust accepted at an early stage that there were serious failures in the care provided to Mrs Cahill and Agnes for which we are truly sorry.
“We are committed to learning from incidents to continually make our services safer.
“Our homebirth service has been remodelled.
“The new service has been shaped by both our own safety investigations and those of the Maternity and Newborn Safety Investigations team, who carried out an independent review.
“We will also study the Coroner’s conclusion very carefully to see if there are any further actions which we should be taking.”