A mother-of-two has been left permanently disabled after waiting nearly two hours for an ambulance when she suffered a stroke.
Susan Harding, 57, has lost the use of the left side of her body after suffering a haemorrhagic stroke at her home in December last year, leaving her with a bleed on the brain.
Her partner, Rob Christensen, 63, says her condition worsened in the time the ambulance took to arrive at their home – one hour and 59 minutes after the first 999 call was made.
The NHS‘s target average response time for category two emergencies – which include strokes – is 18 minutes, with 90 percent of these calls being responded to within 40 minutes.
Mr Christensen said that each time he called back for an update, he was asked to repeat everything from the beginning – which he says made the delays ‘worse’.
He believes the wait caused extra bleeding and pressure on Ms Harding’s brain, which could have been avoided, and told how he was left ‘gobsmacked’ by call handlers’ ‘indifference’.
After the mother-of-two was initially put in an induced coma, doctors told Mr Christensen that she would likely never regain the use of the left side of her body and would need care for the rest of her life.
He is now campaigning for real-time reporting of ambulance response times, an overhaul of call-handling and triage systems to avoid repeated delays, and a clear, time-bound plan for improvements that the public can track.

It took an ambulance two hours to reach Sarah Harding (right), 57, following a stroke when she was at home with her partner Rob Christensen (left)

Ms Harding has been in hospital ever since her stroke on December 12 and has lost the use of the left side of her body
A petition set up by the family calling for an investigation into Ms Harding’s care and changes to the emergency response system has so far gained more than 48,000 signatures.
Mr Christensen, a retired project liaison consultant from Melksham, Wiltshire, said: ‘If the ambulance had been sitting outside our house with the engine running, she still would have had that stroke.
‘But all that extra bleeding and pressure on her brain, a lot of that wouldn’t have happened and she’s now going to be permanently disabled for the rest of her life.
‘We’re supposed to act fast, and we got nothing from the emergency services. For the first time, I felt helpless, really helpless.
‘It’s like a bereavement because she’s not all there. It’s horrible, and it makes me angry – it’s changed our lives.’
Ms Harding suffered the stroke on December 12 while in the bathroom at home, and has been in hospital since.
Mr Christensen said: ‘We had a normal day doing some Christmas shopping and when we got home Susan had asked me to go into the garage to sort some Christmas decorations.
‘Susan was amusing herself, happily sorting through stuff and I was re-soldering battery connections for the wreath.
‘She had gone to the toilet, but five minutes later, she still hadn’t come out, and then I heard a thump against the bathroom door.
‘I found Susan collapsed on the floor.’
Noticing her face had drooped on one side, and her speech was slurred, Mr Christensen leapt into action and called an ambulance – not knowing he’d be waiting almost two hours for it to turn up.
He said: ‘At 16:59, I called it in, and they asked lots of questions – I told them she was having a stroke.

Mr Christensen said delays were made worse by him having to repeat all the details of what had happened to his partner every time he phoned for an update
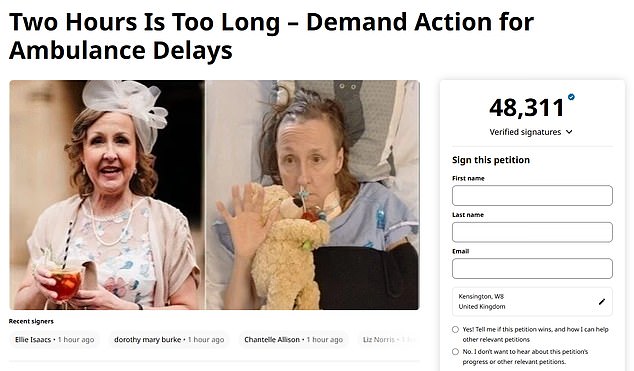
A petition set up by Ms Harding’s family has already garnered more than 48,000 signatures
‘I also called her eldest son, and he made his way over.
‘When he arrived, I phoned the ambulance to chase up – about 50 minutes after the initial call and we had to go through all the same questions again – I couldn’t believe the ineptitude.
‘We’re pacing around, wondering what to do. Do we take her ourselves or wait?
‘By 18:30, it still hadn’t turned up, so I called up again, and they went through the questions again.
‘I was gobsmacked at the indifference. At 18:50, an emergency responder in a car turned up, and then the ambulance finally turned up almost two hours later at 18:58.
‘It was 19:20 before she was finally taken to hospital – by then, the damage was done.’
Ms Harding was taken 14.5 miles to the Royal United Hospital in Bath before being put into an induced coma to be transferred to Southmead Hospital in Bristol – where she remained in an induced coma for nearly four weeks.
She had surgery at Southmead to relieve the bleeding on her brain.
On January 21, 2025, she was moved back to the RUH and eventually to a local hospital in Chippenham for rehab physio in March.
Mr Christensen said: ‘It can take up to 24 months to rehab, but she will need constant physio, and once she’s sent home, they can’t guarantee what treatment she’ll get, if any.

Ms Harding was originally taken to the Royal United Hospital in Bath (pictured) where she was placed in an induced coma
‘It’s horrible, and it makes me angry – it feels like our lives have come to an end.
‘I’m going to be caring for someone that basically isn’t there – she can’t remember things that happened 15 minutes ago.
‘It’s affected her reading and depth of field, and she can’t stand on her own.
‘When I’m not there, she gets anxious.’
Keen to seek answers, he wrote to his local MP and eventually received a letter from the Minister of Health.
He said that other than being busy, South Western Ambulance Service have given no reason for the delay.
He said: ‘Either it’s important to act FAST, or it’s not. If it is, why the hell didn’t the ambulance didn’t turn up within 18 minutes?
‘We’ve all seen the act FAST campaigns on TV – I did act fast and it’s such a disappointment when it doesn’t happen in reality.
‘It’s a lie. This is six-and-a-half times the amount of time we should have waited.
‘You expect better – we’ve been gravely let down, and you expect some tangible response and not something talking about statistics.’
A spokesperson for the South Western Ambulance Service NHS Foundation Trust (SWASFT) said: ‘We would like to offer our sincere apologies to Ms Harding for the delay in our response. The delay was unacceptable and falls below the high standards of care we aim to provide.
‘Delays in our care is not something we want any of our patients to experience, and when a delay does occur, it’s taken very seriously.
‘At the time of Ms Harding becoming unwell in December 2024, our service was under extreme pressure, and our response time was impacted by this. This demand was further compounded by hospital handover delays and system pressures within the wider NHS and social care.
‘We continue to work incredibly hard with our partners in the NHS and social care, to do all we can to improve the service that patients receive.’







