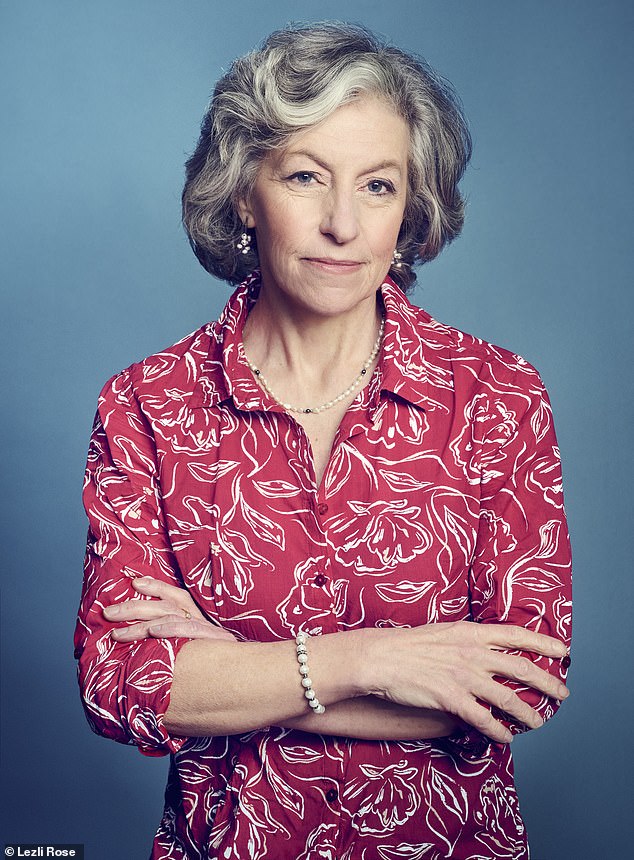
When Helena Burton stopped taking her antidepressant medication she was gripped by a range of intense symptoms: her face went numb, her brain felt ‘like it was being zapped with an electric current’ and her entire world seemed unreal. ‘I felt like I was going mad,’ recalls Helena, 56, a psychotherapist who lives in Essex.
‘Coming off the prescribed antidepressant, venlafaxine, after taking it for 15 years felt like there was a bomb going off in my head. But at the same time I was having doctors shout at me that there was no such thing as antidepressant withdrawal.’
For decades, psychiatrists, GPs and pharmaceutical companies dismissed patients’ claims of severe withdrawal symptoms after stopping antidepressants. Instead, patients were told the symptoms were either imaginary or evidence of their original depression returning.
But in 2019, in the face of compelling research evidence about antidepressant withdrawal, leading medical institutions reversed their previous positions of denial.
After a campaign championed by Good Health, the Royal College of Psychiatrists dramatically changed its stance – now calling for greater recognition of the potential for severe, long-lasting antidepressant withdrawal symptoms.
Since then, the Royal College of Psychiatrists and the treatment watchdog, the National Institute for Health and Care Excellence (NICE), have gone further, recommending that patients who wish to quit antidepressants are supported in slowly cutting down dose sizes over a period of months to minimise the risk of withdrawal effects.
NICE also recommends this tapering approach for withdrawing from two other classes of potentially dependency-forming medicines, the sedative drugs benzodiazepines and widely prescribed sleeping pills known as ‘z’ drugs.
In fact, tapering is important for a surprising number of prescription medicines in order to avoid unwanted side-effects. Anyone given an opioid painkiller for more than two weeks, for example, should reduce the dose by 10 per cent a week or so to avoid withdrawal symptoms, according to NHS guidance.

Helena Burton said coming off antidepressants after taking them for 15 years ‘felt like there was a bomb going off in my head’
Joanna Moncrieff, a professor of critical and social psychiatry at University College London, says ‘withdrawal effects will be much more severe when people have been on the drugs for years’

Anyone given an opioid painkiller for more than two weeks should reduce the dose by 10 per cent a week or so to avoid withdrawal symptoms, according to NHS guidance
Meanwhile, NHS patients prescribed steroid drugs for eczema, asthma, rheumatoid arthritis or inflammatory bowel disease are advised to switch from daily use to every other day for a fortnight, then twice a week for another fortnight and so on, until the drug is completely phased out.
Even blood-pressure pills called beta blockers – taken by millions in the UK – need to be tapered over a 14-day period (sometimes longer) rather than quit suddenly to avoid a dangerous spike in blood pressure.
However, evidence suggests professional support for NHS patients trying to come off some drugs remains patchy, if not virtually non-existent. And many UK medics still appear to be either in denial of or ignorant about the problem.
Last month, a paper by UK psychiatrists in the prestigious journal JAMA Psychiatry used drug companies’ historical research data to claim that withdrawal symptoms are often only in patients’ imaginations.
The paper, by doctors at UK universities and hospitals, concluded that while some individuals may experience symptoms such as dizziness, nausea, vertigo or nervousness, the vast majority do not.
The authors, several of whom declare payments from drug companies, also blamed the ‘nocebo effect’ – where negative expectations cause people to feel worse. It was against such a background that five years ago, Helena decided to stop taking the venlafaxine she was originally prescribed for low mood and negative thoughts.
What jolted her into action was her psychiatrist’s suggested solution for the fact that the drug was no longer working for her. ‘Rather than feeling better, I was feeling steadily worse,’ she says. ‘It got to the point where I was so low I was forgetting how to talk to people or even dress myself some days. My psychiatrist suggested that my depression had now become resistant to the drug and that he would book me in for ECT.’
ECT – or electroconvulsive therapy, where seizures are induced by passing electricity through the brain under general anaesthetic in the hope of treating depression – struck Helena as barbaric.
She decided that stopping the venlafaxine ‘was the only way to get my life back’.
In 2019, Helena cut her prescribed 37.5mg a day (the standard dose) to 7.5mg in the space of a fortnight. But she developed such awful symptoms that she went back to the full dose.
Searching online, she discovered hyperbolic tapering – where you cut your medication down by 5 to 10 per cent every couple of weeks. The smaller the dose becomes the smaller the reduction amounts to, so that towards the end of tapering patients are reducing by tiny amounts.
The problem, as Helena found, is that venlafaxine is prescribed by the NHS only in a coated pill form. ‘Cutting through the coating makes it very difficult to estimate what dose you have created. I had to buy a pill cutter, a weighing machine and used a spreadsheet to record my doses,’ Helena says. ‘The drug is available in liquid form, which is much easier to measure out. But I was told by doctors that the NHS won’t provide it because it is too expensive.’
Despite Helena’s efforts to taper accurately, she says: ‘I did still have some bad reactions at times, such as losing sensation in my arms temporarily. It took me a year to fully taper off my dose and stop in 2021.’
Now off the drug four years, Helena says she feels more emotionally resilient than before.
‘In the past couple of years, I’ve had every cause to feel depressed – including having had a severe accident where I suffered broken bones – but I have not had any symptoms of depression.’ Now she coaches others struggling to come off their prescribed medications.
It should not be this difficult. In 2019, a landmark report by Public Health England – a now-disbanded Department of Health agency – called for the NHS to run a helpline and website to support patients trying to quit psychiatric drugs, after pressure from the All-Party Parliamentary Group (APPG) on Prescribed Drug Dependence, backed by Good Health. Yet nothing appears to have been done about this.
The Royal College of Psychiatrists’ website does now contain advice on tapering, including the warning that ‘no matter how low the dose you get to, you can still get withdrawal symptoms when you stop’. And NICE guidance, introduced in 2023, states: ‘Reducing the dose of antidepressant medication in stages over time helps to reduce withdrawal effects.’
Nevertheless, professional denial of serious antidepressant withdrawal problems remains – highlighted by the recent paper in JAMA Psychiatry.
It effectively minimised withdrawal symptoms, but as Joanna Moncrieff, a professor of critical and social psychiatry at University College London, argues, it covered only short-term consequences of short-term antidepressant use, whereas about 2million people in England have been taking them for over five years.
‘It is completely useless for shedding light on the consequences of long-term use,’ she told Good Health. ‘Obviously, withdrawal effects will be much more severe when people have been on the drugs for years.
‘This study’s main analysis is based on 11 trials. Six of these had people on antidepressants for eight weeks, four for 12 weeks and just one for 26 weeks.’
In contrast, a study she co-authored in the journal Psychiatry Research in May found a clear link between how long someone takes antidepressants for and how likely they are to experience withdrawal symptoms – and how severe these symptoms are.
She says: ‘We surveyed NHS patients and found that people who had used antidepressants for more than two years were ten times more likely to have withdrawal effects, five times more likely for those effects to be severe, and 18 times more likely for them to be long-lasting compared with those who had taken the drugs for six months or less.’
Meanwhile, in the US a new network of specialist clinics called Outro launched last month, co-founded by the UK-based tapering pioneer Dr Mark Horowitz – a clinical research fellow in the NHS who experienced problems withdrawing from these drugs after taking them for 15 years.
When he tried to stop taking antidepressants he suffered from insomnia, panic attacks, dizziness and anxiety. The experience led him to co-develop guidelines on safe withdrawal, published last year as the Maudsley Deprescribing Guidelines.
At his US clinics, for a monthly fee starting at $125 (£93), patients are paired with a clinician who guides them through a tailored hyperbolic tapering programme.
Outro also works with pharmacies to produce custom versions of patients’ antidepressants in minuscule tapering doses.
Dr Horowitz is also co-developing an NHS tapering clinic. He says there is a vast need for support services in the UK. ‘Most NHS clinicians are not educated in how to get people off drugs. That leads to a lot of harm… Many patients I see have tried up to ten times to get off antidepressants and failed because of what are clearly withdrawal symptoms.’
Dr Simon Opher, MP for Stroud and a member of the APPG Beyond Pills – which is campaigning for patients to be helped to withdraw safely from medications – told Good Health: ‘As a working GP I am acutely aware that most GPs have no expertise around deprescribing of antidepressants, tapering or expert advice for stopping safely.’
He is pushing for ministers to implement the recommendation by Public Health England for an NHS-run helpline and website to support patients, but says: ‘I have written to ministers twice about this and still await a response.’
A spokesman for NHS England declined to say whether it was still considering the move, stating: ‘The NHS continues to work with GPs and relevant mental health practitioners to support them in helping patients to make informed choices, tailored to their needs.’
That offers little hope to the millions of Britons parked on antidepressants that they no longer need, but cannot get off without expert support. Drugs that the NHS put them on in the first place.
It took a year for my GP to help me
Kiera Dawes, 25, has fibromyalgia, which causes widespread pain, and four years ago was prescribed gabapentin – known to cause problems for people taking the drug or coming off it.
‘When my doctor first prescribed gabapentin to me, he said there was a lot of research to say it helps with fibromyalgia pain, and that it had few if any side-effects.
‘But not only did it not work for my pain, within weeks I developed brain fog. I’d lose my train of thought and do things like put my phone in the fridge.
‘If I didn’t take my pills bang on time every four hours, I’d feel light-headed, sick and barely able to stand without dizziness. I now know these were withdrawal symptoms.’

Kiera Dawes says ‘even with tapering, withdrawal has been hell’ after she stopped taking gabapentin, which can cause a number of side-effects
Transport coordinator Kiera, from County Durham, adds: ‘The depression and anxiety I’d had before got worse and I went from a size 8 to size 12 in a matter of months, having never had weight problems before. I also developed pain in new places.
‘When I went back to the GP after a month saying gabapentin wasn’t working, they just upped the dose by 100mg a day. And that kept happening which is how, after 18 months, I ended up on 1,200mg a day.
‘I was 17 when I first developed crushing pain in my ribs. My GP prescribed the opioids codeine and tramadol. They didn’t give much relief and left me feeling groggy. After a year, gabapentin was presented to me as a more effective option.’
But last year, Kiera decided to come off the drug. ‘The side-effects were ruining every aspect of my life and had little effect on the pain,’ she says. ‘I hadn’t been able to work for two years. I knew it could be dangerous to just stop overnight. But even though I told my GP gabapentin was doing me more harm than good, no help was ever offered to help me gradually reduce my dose.
‘In March this year my GP put me in touch with a pharmacist at the practice who said she’d ring me every two weeks to find out how I was getting on. She explained that tapering is the safest way to come off gabapentin but warned it could be very difficult. She’s been brilliant, but I only get a five-minute call once a fortnight.
‘Even with tapering, withdrawal has been hell. In the first few weeks I barely ate and had the shakes in my hands. My mood was all over the place. For me, gabapentin is a horrendous drug, and I would never have taken it had I known about its side-effects and the fact that it’s so difficult to come off. There should definitely be more support – it’s a really hard thing to go through.’











