Two of the most commonly taken over-the-counter painkillers could be putting people at risk of stomach ulcers, liver failure and kidney damage, a leading doctor has warned.
Dr Dean Eggitt, GP and CEO at Doncaster Local Medical Committee, warns patients against taking paracetamol, which is also known as acetaminophen in some countries, and ibuprofen anything more than occasionally, saying that they can cause serious harm.
He said: ‘All these simple over the counter medications can actually prove fatal in the wrong doses—and some, like paracetamol, within a week.
‘It’s a huge problem and people just don’t recognise the risk.’
Paracetamol and Ibuprofen—used by millions daily to treat everything from headache to fevers—is safe when taken correctly.
But even slightly exceeding the recommended dose over the course of a week, not just a day, can cause permanent liver and kidney damage, Dr Eggitt warned.
He explained that the danger with Ibuprofen—a non-steroidal anti-inflammatory drug (NAID) used to relieve pain and fever—comes from how the drug is processed by the body, irritating the stomach lining and increasing the risk of stomach ulcers.
‘Painkillers like Ibuprofen are designed to relieve inflammation, but really all they do is irritate the stomach, increasing the risk of painful stomach ulcers which in some cases can lead to peritonitis.’

Ibuprofen is taken by millions to reduce inflammation and ease pain, but Dr Eggitt warned that prolonged use could mask symptoms of infection
Peritonitis occurs when the lining of the stomach becomes infected, which can be caused by heavy painkiller use.
Left untreated the condition can be life threatening. The peritoneum covers internal organs including the kidneys, liver, and bowel, which can become damaged when the lining is infected.
This is most often caused by a burst stomach ulcer—which can result from regular use of anti-inflammatory painkillers.
Dr Eggitt added: ‘I can’t remember the last time I took an over-the-counter painkiller like Ibuprofen—it’s terrible stuff.
‘The other problem with painkillers is that it often masks the real problem, delaying diagnosis for what can be a sinister underlying health condition,’ he continued.
And when it comes to paracetamol, his verdict was much the same.
He explained the problem lies in the way people take paracetamol and how it is processed by the liver.
‘People think paracetamol is harmless because it’s easy to get so people take it like Smarties. But even if you’re not exceeding the recommended amount in one day, you can still overdose,’ he said.

Over the counter painkillers, like paracetamol, are used by millions of Britons everyday to deal with headaches, muscle pain, or fevers—but can cause permanent damage to the liver
When paracetamol is broken down in the body, it produces a by-product called NAPQI.
At low doses, this toxic waste-product can be neutralised by a protective substance called glutathione.
But at high doses the liver can become overwhelmed—leading to permanent liver failure, caused by a delayed overdose.
There is growing concern about the soaring number of cases of liver disease, which have surged by 40 per cent over the past two decades.
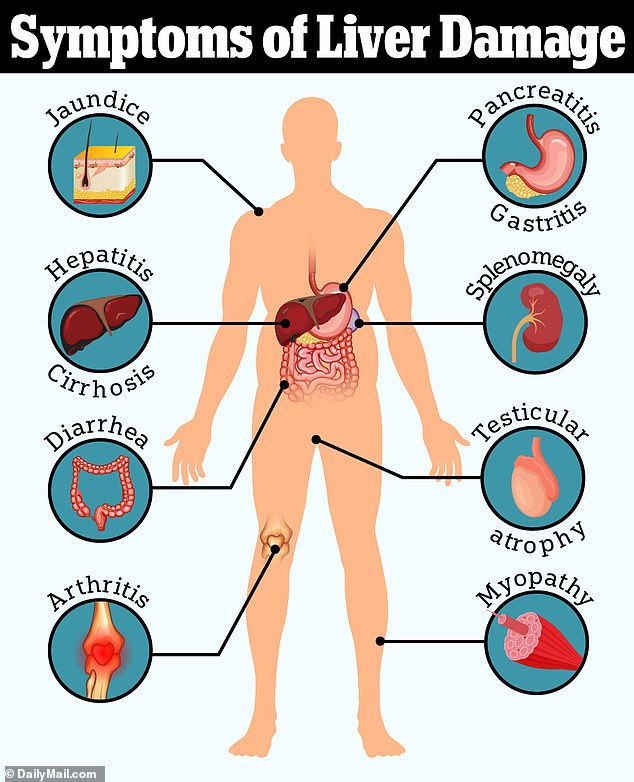
Dr Eggitt said: ‘We too often see people presenting with jaundice—a tell-tale sign of liver damage—triggered by a delayed overdose, where patients may have taken up to 10 paracetamol a day for week, exceeding the recommended dose.’
Left untreated, severe liver damage and scarring can lead to cirrhosis, leaving patients in need of a liver transplant.
Another commonly prescribed over-the-counter medication that Dr Eggitt takes issue with is Loperamide—a drug used to treat diarrhoea.
It can offer immediate short-term relief, reducing the number of times someone needs to use the bathroom and firming up stool.
It works by slowing down digestion, allowing the body to absorb more water from the intestines.
However, Dr Eggitt warned, long term use could actually be masking the symptoms of bowel cancer, which can be fatal, especially when diagnosed at the later stages.
‘People who rely in loperamide may actually be making bowel cancer, delaying potentially life-saving treatment until it is too late,’ Dr Eggitt explained.
Around 90 per cent of bowel cancer patients who catch the disease early and are diagnosed at stage one will survive their cancer for five or more years.
But once the cancer has spread, the prognosis is much bleaker with only 10 per cent of patients diagnosed at stage four surviving at least five years after their diagnosis.
Bowel cancer is the second biggest cause of cancer deaths in the UK, with 16,8000 people in the UK dying from the disease every year.
And cases seem to be rising in under-50s.
While the disease has long been linked to obesity, experts have noted that the cancer also seems to be affecting fit and healthy individuals.
As such, some experts have blamed environmental factors that young people have been exposed to more than previous generations, including ultra-processed foods, microplastics and even exposure to E.coli in food.
There are around 2,600 new bowel cancer cases in people aged 25-49 people in the UK every year—and around 44,100 new cases among all ages.
Overall, just over half of bowel cancer patients are expected to be alive 10 years after their diagnosis.












