The slide into addiction and despair was frighteningly easy.
It all began when father-of-one Grant Smith* was facing redundancy from his job in music events management, and then lost his mother within few months.
The 58-year-old from Somerset began to drink heavily, at first searching for something to numb the unhappiness he felt.
Rapidly, one or two glasses became a bottle a night, and he says he simply lost control.
‘I’d always enjoyed a drink, but things began to spiral. I worked from home, and at odd hours, so I fashioned a life where it appeared that I was functioning – but the drink was starting to take over,’ he admits, recalling the episode in 2019.
‘Eventually, I went to the GP and explained my problems, hoping for some kind of support or treatment. But he said that I was “not drinking enough” to get referred for professional help.
‘I had managed periods where I’d stop drinking before but the urge always returned, and this time much stronger, I couldn’t just stop myself,’ says Grant.
‘To everyone else I was fine, I could hold down a job, even run marathons, but it was the drink that was helping me get through the day.

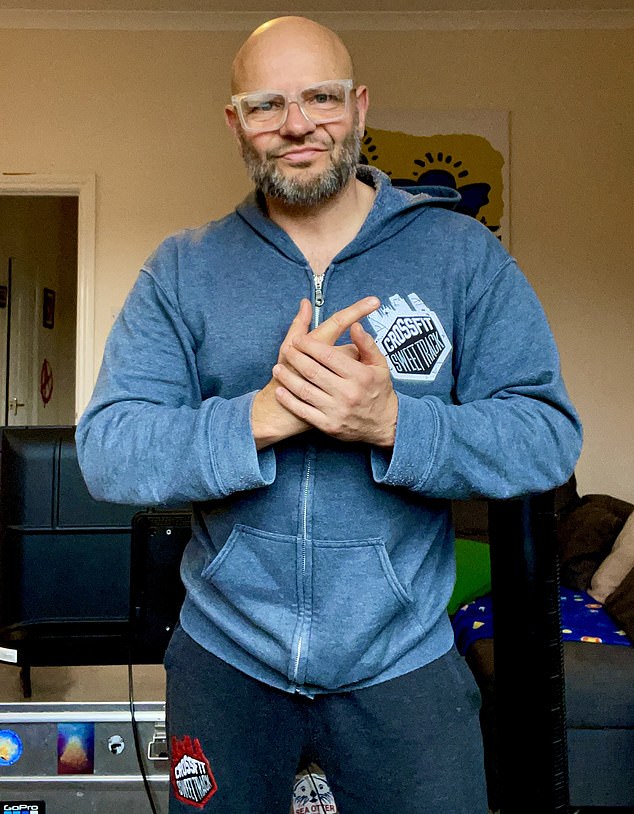
58 year-old Grant was told by his GP that he wasn’t drinking enough to qualify for professional help
The father-of-one enrolled on a groundbreaking trial run by the University of Exeter to help overcome his drinking problems
‘As a dad I had hated what I had become, and I was getting sick of myself, it was my dirty little secret and I knew it had to stop.’
Then, by chance, Grant came across a Facebook advert looking for volunteers to take part in a medical trial for a new drug treatment for alcohol addiction. He signed up – and, in his own words, ‘it changed everything’.
Four years later, he’s sober and no longer feels the urge to drink.
So what was the therapy that brought about such a remarkable turnaround?
It was ketamine – a powerful medical anaesthetic better known for its reputation as a party drug. Infamously abused for its hallucinogenic effects, ketamine has become one of the fastest rising substances of misuse in the UK.
While overall drug use is falling, ketamine use is climbing – particularly among young people. Campaigners have warned that taking it is now seen as ‘almost a rite of passage’.
The drug was also linked to the death of Friends star Matthew Perry, who is believed to have first been prescribed it to treat depression and anxiety.
But the version Grant received was arketamine – a pharmaceutical formulation now being explored as a possible breakthrough in treating heavy and dependent drinkers.

Four years on from the ketamine treatment Grant is still sober, and says he does not feel the urge to drink
As part of a clinical trial run by scientists at the University of Exeter, participants were given three infusions of arketamine alongside a course of cognitive behavioural therapy (CBT) – the gold-standard treatment for alcohol misuse.
Another group received CBT alone, paired with placebo infusions.
To qualify, volunteers had to be diagnosed with severe alcohol use disorder – typically defined as drinking around 150 units per week – the NHS recommends drinking no more than 14 units per week.
Early results have been striking. Those given the ketamine-therapy combo went from drinking daily to remaining sober 86 per cent of the time over a six-month period – significantly outperforming the therapy-only group.
Experts believe that the drug works because in part it combats the depressive mood created by alcohol use disorder.
It does this by increasing levels of a substance called glutamate, which helps brain cells function better.
Previous studies have suggested that arketamine is more effective than standard antidepressant medication for treatment resistant depression.
‘Depressive mood can often lead to relapse,’ says Professor Celia Morgan, an expert in psychedelic research from the University if Exeter. ‘When people turn to alcohol they are often self medicating for depression, which is why when there is a sudden stop their depression can get worse which is why we currently see high levels of relapse.’
Crucially, during the trial, each cognitive behavioural therapy (CBT) session was scheduled within 24 hours of an intravenous dose of arketamine.
‘The timing of the CBT is key,’ explains Professor Morgan, who led the study. ‘The drug induces a period of heightened neuroplasticity – when the brain is more open to change.
‘Patients become more receptive to learning, which makes the therapy significantly more effective.’
Arketamine treatment isn’t without side effects, however. Alarmingly, Grant explains that after the first infusion he experienced hallucinations over the course of the 45 minute treatment.
It was after the second transfusion that he felt the transformative effect.
‘I just let go,’ said Grant. ‘It felt like my soul had left my body, it felt like I was looking down on myself, I lost the feeling of everything around me. It was really profound.’
Since completing the trial, Grant says he hasn’t felt the urge to drink at all.
Unlike previous attempts at sobriety, he’s now able to be around alcohol – at home or social events – without any temptation to relapse. Notably, he hasn’t needed any further therapy or support in the four years since his treatment ended.
Researchers behind the trial say the main benefit of this approach is its ability to dramatically reduce relapse rates.
Current data suggests that up to three in four patients with severe alcohol misuse disorder relapse after conventional treatment. By contrast, early findings from the ketamine-CBT combination are significantly more encouraging.
Alcohol misuse costs the NHS an estimated £4.9 billion a year. According to NHS Digital, alcohol-specific and alcohol-related hospital admissions rose in the most recent year on record (2023-24), with the rate for alcohol-related admissions now at its highest since 2016.
Professor Morgan said: ‘The trial data has shown that it is really effective at preventing relapse within six months, but we have had patients where it has been effective for four years without further treatment.
‘The impact of dealing with relapse would be huge, preventing serious damage to patients’ lives and also saving the NHS considerable money as these same people will not end up back in A&E or addiction services.’
The hope though is that the treatment will be available across the NHS in the near future following successful trial data.
The research has found that the only common side effect is a raising of blood pressure, which experts say could limit the number of people who are eligible for the treatment.
Dr Christos Kouimtsidis, consultant psychiatrist in addictions at Surrey and Borders Partnership NHS Foundation Trust, which took part in the trial, said: ‘Since the pandemic, we’ve seen a growing number of people referred to our services for support.
‘The hope with this treatment is that it will reduce relapse rates, meaning fewer people need to return for ongoing care – helping both patients and easing pressure on the service.’
*Grant’s name has been changed for anonymity












