How much you’re spending on taxes could influence your risk of cancer, a study suggests.
Researchers found a link between states with high tax rates and a reduction in deaths caused by cancer.
For every additional $1,000 generated through tax revenue per person each year, the death rate from cancer decreased by up to four percent.
High tax states like New York, Connecticut and New Jersey had some of the lowest mortality rates in the country, while those with less income tax like Mississippi, Tennessee and and Kentucky were among the worst.
The researchers say the reason is high tax states are more likely to offer screening and other tests to catch cancer at earlier stages.
For every additional $1,000 in tax revenue, cancer screening rates generally increased by up to two percent, the study found.
The researchers – from Ohio State University, Emory University in Atlanta and University of Verona in Italy – said better outcomes for states that pay more taxes could be because those taxes are funding screening methods like mobile testing sites.
However, there were outliers. Utah, for example, had the lowest cancer mortality of any US state and was also among the lowest tax states. Utah’s lower cancer rates could be in part due to a lower prevalence of tobacco and alcohol, both of which are shown to cause cancer, and other lifestyle choices in the heavily religious state.

A new study suggests paying higher taxes lowers the risk of dying from cancer and improves the chance of getting screened (stock image)
The researchers wrote: ‘Designing tax systems based on high tax revenue and progressive policies may present one aspect of a multifactorial approach to improve cancer-related outcomes, thus mitigating persistent cancer health care inequalities in the US.’
The study, published Friday in JAMA Network Open, combed through data from the US Census Bureau and the Institute on Taxation and Economic Policy to calculate the average tax revenue per person in each state and how much rates have changed over time.
Tax revenue was calculated from 1997 to 2019.
The researchers also evaluated cancer mortality data from 1991 to 2021 using CDC databases.
Cancer screening rates were calculated from 2020 to 2022.
The average cancer mortality rate for 2021 was 174 deaths per 100,000 white Americans.
In the non-Hispanic Black population, however, the mortality rate jumped up to 206 per 100,000.
Kentucky had the highest overall cancer mortality rate at 205 per 100,000 people, while Utah’s rate was lowest at 133 deaths per 100,000 people.
Over the course of 23 years, the average national state tax revenue per person per year was $4,432.
New York had the highest tax revenue per person at $8,400 with Connecticut and New Jersey following closely behind at $7,100 and $6,800, respectively.
All three states had a cancer mortality rate of 160 to 168 per 100,000 people, below the national average.
The lowest tax revenue was found in Alabama ($3,300), with Tennessee ($3,400) and Mississippi ($3,500), South Carolina ($3,500) and Idaho ($3,500) following.
Mississippi had the second highest cancer mortality rate at 201 per 100,000 people. Rates in Tennessee and South Carolina were 193 and 184 per 100,000 people, respectively.
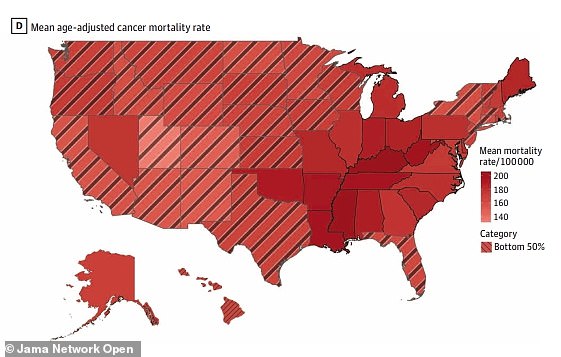
The above map shows the average cancer mortality rate per state. Kentucky had the highest, which was closely followed by Mississippi
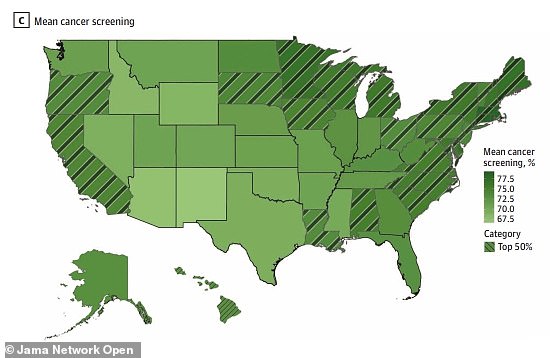
The above map shows the rate of cancer screening. Rhode Island consistently had the highest screening rates, while Alaska and Arizona had the lowest
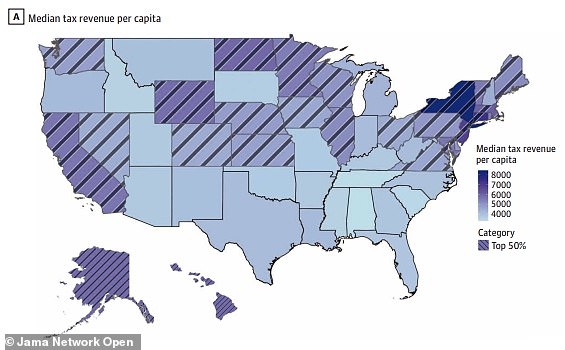
The above map shows the average tax revenue per capita in each state. New York, Connecticut and New Jersey all had the highest tax revenues
The researchers found that for every $1,000 tax increase, cancer mortality for all cancers decreased by two percent on average. The decrease was even greater, three percent, for white individuals.
For cancers with recommended screening like colon and breast cancer, each $1,000 tax increase per capita was associated with a four percent decrease in mortality rate. This increased to five percent for white populations.
The researchers said this could be due to increased tax amounts funding state health initiatives and screening measures.
These may include mobile testing sites, subsidizing the cost of transportation to a screening test or offering financial incentives for screening.
Utah, however, had the lowest cancer mortality rate but also ranked among the lowest in taxes at $3,800 per capita per year.
While the researchers did not provide an explanation for this, the lower risk of death could be due to less prevalence of common risk factors.
In 2022, the latest data available, Utah had the nation’s lowest smoking rate at seven percent.
Smoking is responsible for about nine in 10 cases of lung cancer, which causes the most deaths of any other cancer in the US.
Additionally, 12 percent of adults in Utah binge drink, which is considered four or more drinks in one sitting for women and five for men. This is the lowest percentage in the US.
Alcohol has been shown to increase levels of hormones like estrogen, a main driver of breast cancer. It also damages cell DNA, leading cells to grow out of control, raising the risk of them becoming cancerous.
The lack of smokers and drinkers may be due to Utah’s high percentage of Mormons, a religious group that shuns both habits. More than half of Utahns identify as Mormon.
The researchers wrote: ‘These evidence-based screening programs represent successful state-level initiatives and should highlight how government allocation of revenue can advance health care and cancer prevention goals.’
However, there were no notable differences between tax increases and cancer death for minority populations. This suggests increased screening measures have not reached minority groups.
There were several limitations to the research, including the data showing an association between taxes and cancer rather than a direct cause.