Recently, my Apple Watch has been waking me up warning that my heartbeat is below 40 beats per minute. Should I be worried? I’m a 75-year-man who exercises and my only vice is that I drink a few bottles of wine a week.
Smart watches are notoriously unreliable during sleep. However, excessive alcohol consumption can also be the cause of a low pulse.
These devices can be useful for providing helpful health data, including your daily step count, and sometimes spot serious problems such as atrial fibrillation – a heart rhythm problem.
However, they are not medical devices, meaning they are not always accurate. I also would not recommend sleeping with one on.
This is because heartbeats can fluctuate in the night. The average pulse is about 60 to 90 beats per minute, but, during sleep, it’s normal for it to drop to 40 beats per minute. This can be alarming to a smart watch – which will often send a health warning to the user – but it’s nothing out of the ordinary.
A low pulse is usually only a problem if it occurs during the day and leads to dizziness, tiredness, fainting and/or shortness of breath. This is called bradycardia and can occur after a heart attack or due to thyroid disease or sleep apnoea (where breathing becomes obstructed during the night).

Smart watches can be useful for providing helpful health data. However, they are not medical devices, meaning they are not always accurate
In some cases, it can also be triggered by excessive drinking because alcohol can, in severe cases, damage the heart. The NHS advises no more than 14 units a week – about one and a half bottles of wine. Consuming multiple bottles a week will increase the risk of heart problems as well as other issues such as liver disease and cancer.
Anyone concerned about their heart rate should speak to their GP, who can arrange a 24-hour monitoring of the pulse via a portable device.
My prostate is enlarged and is causing me problems when going to the toilet. What can I do that doesn’t involve surgery?
It is very common for an enlarged prostate to be treated without surgery. There are several drugs that can help relieve symptoms.
Prostate enlargement is a common problem among men aged 50 and older. Over time, the prostate naturally grows and can eventually lead to urinary problems including a weak stream, urgency, starting and stopping, straining to push out urine as well as going very frequently and feeling like you have not fully emptied your bladder. Patients may also start passing water several times a night, disturbing sleep.
Anyone who experiences these symptoms should see their GP, as cancer needs to be ruled out. However, in most cases it will be due to an enlarged prostate.
Alpha blockers are commonly prescribed. These tablets, such as tamsulosin, reduce some of the more bothersome issues.
Another possibility would be a tablet called finasteride, which can help reduce the size of the prostate. It isn’t suitable for everyone, however, and can lead to erectile dysfunction. It may also take six months to work.
Only if medication fails or where side-effects are severe – for instance, where patients cannot go to the toilet at all – would surgery be considered.
The procedure, called transurethral resection of the prostate, or TURP, involves inserting a surgical instrument up through the penis and trimming away excess tissue. It’s typically performed under general anaesthetic and requires at least one night in hospital. It is highly effective and complications are rare.
I have agonising diverticulitis. I get these attacks that can last hours but I’ve been told I’m not an urgent enough case to warrant surgery. What should I do?
Diverticulitis is where tiny little sacs develop in the wall of the bowel. These pockets can become inflamed and even infected, leading to stomach pains, nausea, weakness and bleeding from the back passage.
It is thought to be linked to a low-fibre diet, so what you eat is crucial for combating painful symptoms. Roughly nine in ten Britons fail to get enough fibre, so diverticulitis is increasingly common – particularly among those over the age of 50. Smokers and those who are obese are also more at risk.
In severe cases, surgery might be required, but this would only be offered if patients are regularly hospitalised with serious infections. Antibiotics are also offered, but cannot treat the underlying problem.
Instead, most diverticulitis patients need to up their fibre intake. Fibre is found in nuts, seeds, wholegrains, oats and root vegetables. It can also be taken as a supplement.
However, boosting fibre consumption must be done gradually. This is because a sudden increase can lead to bloating and wind – both of which can inflame diverticulitis. This is why GPs generally advise not increasing fibre intake during a flare-up.
Patients should also drink more water, lose weight, quit smoking and avoid red meat. Regular exercise may help, too.
HRT isn’t the only answer…
Research this week from Cambridge University showed that menopause is linked to reductions in grey matter in key brain areas that affect mood and reaction times. I found this interesting given the backlash from campaigners about antidepressants during menopause – something I’ve never fully understood, other than as a sign of the lingering stigma around mental ill health.
Anxiety and depression can absolutely be features of menopause. And both US and British regulatory bodies recommend antidepressants as a treatment for this aspect of the transition. This isn’t a fob off – it’s evidence-based medicine. I’m a fan of HRT when women need it, and for many it’s life-changing. But this data should put a halt to the more sweeping claims that HRT prevents ageing, protects against dementia, or is the only treatment a menopausal woman may need.
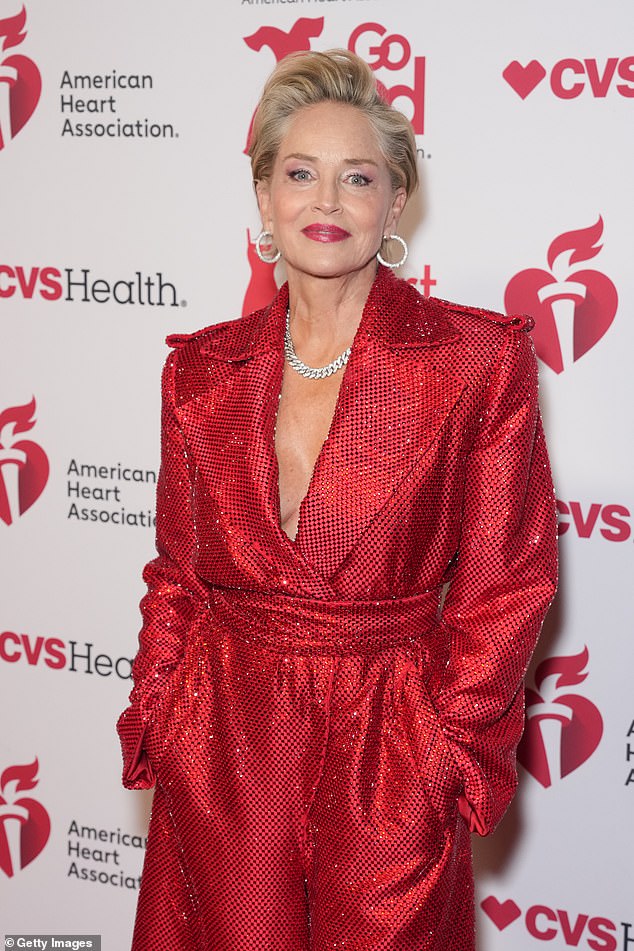
There are endless celebrity examples – like Sharon Stone, 67 – who look fabulous for their age, but I have patients who look and seem both younger and older than they are.
Are you a super-ager like Sharon Stone?
Are you bothered about ageing? I’m not particularly – in the wrinkles and grey hair sense.
But I would like to stay as healthy as possible for as long as I can, so I am intrigued by the different rates that ageing affects people. Of course, there are endless celebrity examples – from A-listers Sharon Stone, 67, to Jane Fonda, 88 – who look fabulous for their age. I was gobsmacked to learn Jeff Goldblum, star of Wicked, is 73. But I have patients who look and seem both younger and older than they are.
Lots of the talk about biological ageing is, frankly, health fiction. But there must be an explanation for why some really do seem to age so much slower. I suspect it is all in our genes. I want to know what readers think. Do you look far younger? Write in to let me know.
Do you have a question for Dr Ellie Cannon? Email DrEllie@mailonsunday.co.uk