Every year, on a quiet September morning, Katie Mitchell pauses before the day begins, giving silent thanks for the extraordinary gift that saved her life: a heart and double lung transplant when she was just 15 years old.
It is not a date circled on any public calendar, yet for Katie, from Sidcup, south east London, it carries a weight greater than birthdays or holidays. It is the day she was given a future.
Last month marked 38 years since that operation. In the extraordinary world of transplant medicine – where success is never promised, survival can sometimes be counted in years rather than decades, and rejection is a lifelong threat – Katie is now believed to be the longest surviving heart and lung transplant recipient in the UK.
‘It’s hard to explain how that makes me feel,’ she said of this poignant record.
‘Every anniversary is bittersweet, because, obviously, I’m so glad I’m still here, but it’s the time you think about your donor the most – you can’t ever lose sight of the fact that your life has been enabled by the loss of another.’
Even more extraordinary is the fact that Katie has also survived two kidney transplants – one in 1994 and a second in 2014 – making her one of only a handful of people in the country to have received four transplanted organs.
Not that you would guess the astonishing medical hurdles Katie, now 53, has jumped in order to be where she is today: an operations manager for a tech company, she looks – remarkably – like anyone else going about their daily business.
While she takes a cocktail of pills to prevent rejection – some of which cause weight gain and fluid retention – she says that day to day she hardly ever thinks about what she went through.

When doctors discovered what was wrong with Katie (pictured) the only treatment option was a heart and lung transplant
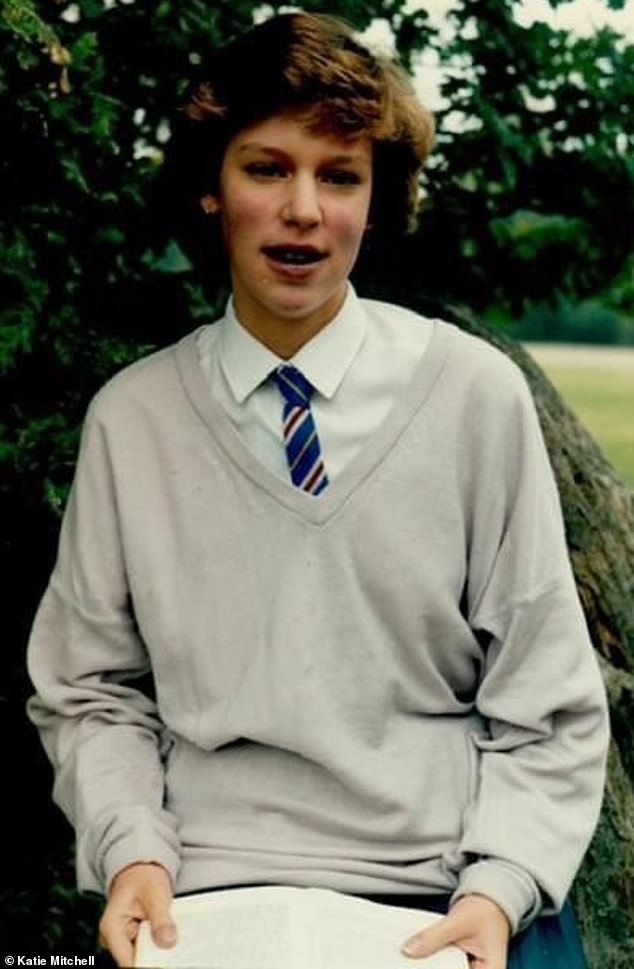
Katie Mitchell is pictured aged 15, a couple of months before her operation. Her lips appear blue due to lack of oxygen
‘I don’t ever take my health for granted, of course. but I don’t live in a bubble,’ she said. ‘I live my life. To do anything else would be a disservice to myself and to my donor.’
Katie grew up with her parents and younger brother in what she describes as a happy, ordinary childhood.
From her early years, however, something seemed slightly off. Exertion often left her breathless for longer than her peers, and after her worried parents took her to the doctors she was diagnosed with asthma.
Yet inhalers did not seem to help, and as she got older, her breathing problems worsened.
With her parents’ concern mounting, she was referred to specialist consultants at the age of ten and, after months of tests and observations, the devastating diagnosis came: Katie had Eisenmenger syndrome – a complex, irreversible condition caused by an untreated hole in the heart she’d had from birth but which no one had spotted.
It leads to high blood pressure in the lungs, causing permanent damage to both the heart and lung tissue.
In the 1980s, when Katie was diagnosed, there was almost no effective treatment.
‘Today, medicine has advanced so much that if I was born now, it would have been spotted and a simple procedure could have sorted the problem,’ she said.
Back then, however, the prognosis was brutal: Katie’s heart and lungs were failing and, without intervention, she would not survive into adulthood. The only option – the only chance – was a heart and lung transplant.
With the passage of time, Katie said she cannot remember how this news was broken to her, or her parents’ reaction.
But one can only imagine their fear – 38 years ago, heart–lung transplantation was still in its infancy. The first successful procedure in the UK had been performed just four years earlier, in 1983, by pioneering surgeon Sir Magdi Yacoub, and few other case studies existed.
How does a young girl even begin to cope with this terrifying prospect? Katie said she was pragmatic.
‘There was simply no alternative, so while it was a huge thing to face, the transplant was something to hang on to, the thing that could make me better,’ she recalled. ‘Maybe it was the naivety of youth, but I just never thought it wouldn’t happen or that it wouldn’t work.
‘I think it helps that this was pre-internet and Google, so I just had to rely on the information given to me by the hospital.’
Katie was referred to the Royal Papworth Hospital in Cambridgeshire – then one of only two hospitals in the country performing heart–lung transplants – and spent a week undergoing rigorous assessments: scans, blood tests, cardiac monitoring and lung function studies.
‘I remember answering lots of questions which I think were about whether I could be mentally prepared,’ she said.

Katie has said that there is a strange contradiction in receiving transplanted organs: she said ‘you want the phone to ring, because it means your chance has come. But you also know it can only ring because someone else has died’
At the end of that week, she was told she would be placed on the transplant waiting list – but it would be another two years before the call came that would change her life.
It is, as Katie explained, a kind of suspended existence. Transplants require a donor whose organs are a match in size, and because the heart and lungs must come from the same donor, they are extraordinarily rare. Even today, only around five such operations are carried out in the UK each year.
‘You live with a strange contradiction,’ Katie said. ‘You want the phone to ring, because it means your chance has come. But you also know it can only ring because someone else has died.’
Her health deteriorated steadily during the wait. ‘I had to think about every breath I took,’ she said. ‘To get to the top of the stairs could take me ten or 15 minutes, and if I needed to get something from another bit of the house I had to plot the route to make it the shortest way.’
As time moved on, her condition took a further toll. She lost so much weight she dropped to five stone and her fingers and lips turned blue from lack of oxygen. Unable to go to school in her final months before the transplant, she could only look on as her friends lived a life denied to her.
Then, one autumn afternoon in September 1987, the call came.
‘It was a pager in those days,’ Katie said. ‘I was at home having my hair cut when it went off. Mum rang the hospital, and they told us to get to Papworth immediately.’
The waiting was over – but a frightening new chapter lay ahead. ‘It’s something you’ve been waiting for for so long, but it’s also very scary to have the operation and you also know something bad has happened to another family,’ Katie said of the maelstrom of emotions that gripped her.

Being the recipient of four organs meant that pregnancy was too risky for Katie (pictured) and so she decided not to have children – a tough decision as she had always wanted to have them
Whisked into theatre on arrival at the Royal Papworth, Katie underwent a gruelling eight-hour surgery, coming round in intensive care to the miracle of being able to breathe without thinking about it.
‘It was incredible,’ she said. ‘Obviously my chest was really painful, but just being able to breathe without effort was amazing. Everyone remarked on the fact that my lips were pink for the first time in a long time.’
The weeks after transplant surgery are a battle zone. In the 1980s and 90s, more than a quarter of heart-lung patients died in the first 30 days after surgery. Immunosuppressant drugs are essential to prevent rejection of the new organs, but the doses must be constantly adjusted. The threat of infection looms.
Katie stayed in hospital for six weeks as doctors measured her medication and blood. She underwent extensive rehabilitation, and when she had regained enough strength to walk again, she was moved into a nearby rehabilitation flat to learn how to take care of herself.
But four weeks in, she suddenly began struggling for breath – a sign of organ rejection. She was rushed back to a high-dependency ward and placed on powerful steroids and intravenous treatments until her body stabilised.
‘It was frightening,’ she said. ‘But I never believed it wouldn’t work.’
Finally, not long before Christmas, Katie was discharged to start her life anew. ‘It’s lovely to be home, but it’s also a little bit scary, because you don’t have that support on call,’ she said. ‘In hospital you can rely on the doctors, but now it’s down to you to remember to take your medication and look after yourself.’
She attended hospital three times a week for biopsies and blood tests, then twice weekly, then monthly. By January 1988 she was well enough to return to school, and went on to take both GCSEs and A levels.

Katie said she is ‘grateful beyond belief for the decades of life given to her by a stranger’ via organ donation.
Along the way were milestones, not least the first anniversary of her surgery. At this stage, even now, just over half of heart–lung transplant patients are expected to survive beyond 10 years, according to NHS figures. Back in the 1980s the figure was half that, at just 26 per cent.
Yet Katie never saw herself as a statistic. She saw herself as someone who had been given a chance – and she intended to use it.
‘There’s this temptation to wrap yourself in cotton wool,’ she said. ‘But what would be the point of surviving if you’re not going to live?’
Even as she embraced life, however, the shadow of her medical past never disappeared entirely.
In her late teens, a routine blood test revealed her kidneys were deteriorating – a known side effect of the strong anti-rejection drugs she needed to survive. She needed a kidney transplant and thrice weekly dialysis in the meantime.
‘It was a huge blow,’ she said of the devastating news. ‘Because it was only at that point that I was starting to feel a lot better and be more independent, so it felt like going backwards.’
Again, Katie had to wait for a vital call, which came three years later, when she was 22. Once recovered, she began to carve out the life she wanted, working in different career roles, including at the Post Office. She moved into her own place, and not long after her transplant, met Lex, the man who would later become her husband.
But yet again, life delivered another blow. When she and Lex began talking about starting a family, Katie sought medical advice. Her heart and lung function were stable, but sadly the risks of pregnancy – intensified by her kidney transplant and medication – were high. ‘When I met with an obstetrician and a renal consultant they advised me not to start a family,’ she explained.
As her 30s progressed, watching her friends have children was ‘really hard’, she acknowledged. ‘I always wanted kids, and I had always imagined I would be a mum. I think for myself I would have taken the risk, but Lex didn’t want me to and I understood that.’
Her kidney lasted 18 years before it started to fail, meaning that once again Katie had to return to the brutal timetable of three dialysis sessions per week, each lasting four hours – ‘it’s like having a part-time job,’ she joked. In 2014, she received a second kidney transplant at Guy’s and St Thomas’ Hospital.
Today, Katie remains pragmatic about her survival, even if, over the years, she has seen others who have undergone transplants subsequently lose their battle for life.
‘Being a transplant patient means you join a strange little club,’ she said. ‘You get to know people who have travelled the same path and even if you don’t know them well, it is very hard when things don’t work. You don’t really know them in depth, and you don’t know their families, but it hits you quite hard because you’ve had the same operation.’
It’s why she is determined to make the most of her life, marching forward through medical territory she acknowledges is uncharted.
‘Of course I would much prefer there were a lot of people who’d had transplants for a lot longer than me, but I try not to think about that side of it,’ she said candidly. ‘I just try and live my life and be grateful for the fact I am still here.’
Organ donation has changed since Katie’s transplant in 1987. In England, Scotland and Wales, adults are now automatically considered organ donors unless they choose to opt out. But families still have the final say, which is why Katie is urging those who have not opted out to be clear about their wishes.
‘It’s so important to talk about organ donation,’ Katie said. ‘Tell your family what you want. One donor can save several lives. I’m here – 38 years later – because someone said yes, and their family gave their blessing.’
Today, there are more than 8,000 people waiting for an organ transplant in the UK. Last year, 460 people died while waiting.
Katie knows she could have been one of them. And she is grateful beyond belief for the decades of life given to her by a stranger.
To find out more, and confirm your support for organ donation, call 0300 123 23 23, visit organdonation.nhs.uk, or use the NHS app.












