NUTRITIONIST Rob Hobson was told he had a condition which, left untreated, can lead to a heart attack… He had no idea, and neither do millions of Brits with the same disorder.
He warns that the ‘silent killer’ is clogging up arteries across the country and worldwide, even in people leading a healthy lifestyle, just like him.
The statistics are hard to ignore – every five minutes, someone in the UK is admitted to hospital due to a heart attack; strokes claim 34,000 deaths each year; and heart disease remains our biggest killer, taking 180 people’s lives every single day.
Last week, the Global Burden of Disease study warned that globally, cases and deaths of heart disease, also known as cardiovascular disease (CVD), are surging, blamed on increasing rates of obesity and diabetes.
One of the biggest drivers behind heart disease is high cholesterol, known as the ‘silent killer’ because there are no obvious signs or symptoms.
In fact, the first sign it exists is a heart attack or other serious cardiac event. And by then, it can often be too late.
It’s estimated that up to half of Brits have cholesterol levels exceeding a healthy limit, according to the British Heart Foundation.
Dr Oliver Guttmann, consultant cardiologist at The Wellington Hospital (part of HCA Healthcare UK), says: “You can feel completely well and still have cholesterol levels that increase your risk of heart attack or stroke.
“For the vast majority, there are no obvious warning signs.”
So, the question is, would you know if you had high cholesterol?
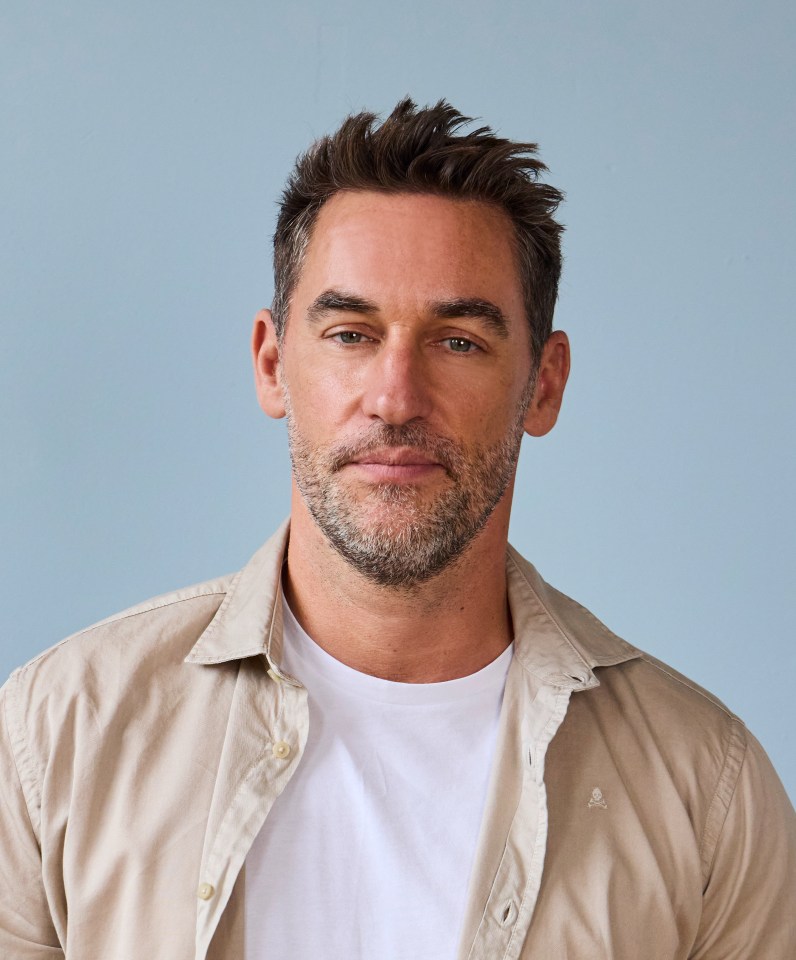
Rob Hobson, a 47-year-old from Brighton, was dumbfounded by his diagnosis.
As a nutritionist, he’s an advocate of good health.
Rob tells Sun Health: “If it can happen to me, how many other seemingly healthy people are walking around with high cholesterol?
“Even if you feel great and eat well, it’s still worth knowing your numbers. High cholesterol doesn’t have symptoms, and you can’t manage what you don’t measure.”
Here, we reveal how to find out YOUR numbers, and the best way to get it down fast…
What is cholesterol, and how can I get mine tested?
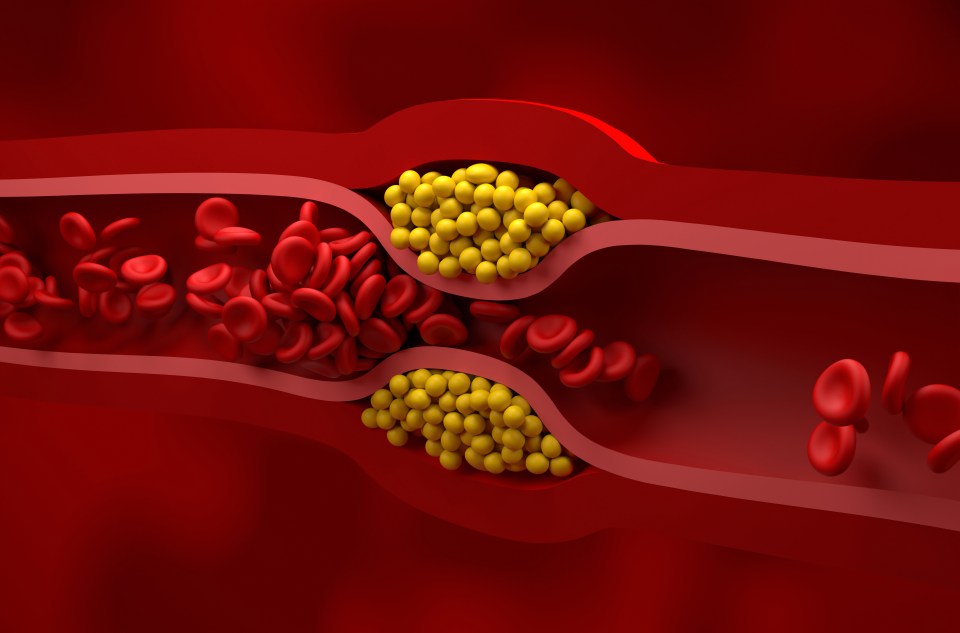
Cholesterol is a fatty substance in your blood, produced primarily in your liver.
Dr Guttermann says: “Your body needs small amounts of cholesterol, but too much can be dangerous.
“LDL, known as ‘bad’ cholesterol, can build up as plaque in your arteries, known as atherosclerosis, making them narrower and raising the risk of heart disease and stroke.
“HDL ‘good’ cholesterol helps clear cholesterol away.”
It’s vital to ‘know your numbers’, which means getting your cholesterol checked to see if it’s within a healthy range.
You can ask your GP for a cholesterol test, but you can also buy them online these days. For example, the Healthy Heart Check by PocDoc test (£40, Pharmacy2U).
From the age of 40, your GP should also invite you for an NHS health check once every five years. During this check, your cholesterol will be tested.
Dr Guttmann says: “Cholesterol testing involves a simple blood test.
Your total cholesterol should ideally be below 5.0 mmol/L (millimoles per litre, the unit used to measure the concentration of substances in blood).
Dr Gutternmann adds: “LDL (bad) cholesterol should be below 3.0 mmol/L, and HDL (good) cholesterol should be above 1.0 mmol/L for men and 1.2 mmol/L for women.”
Risk factors include being overweight, high blood pressure, smoking and/or diabetes.
Most healthy adults are advised to have their cholesterol checked at least once every five years
Dr Oliver Guttmann
But Rob’s dangerous levels of cholesterol were actually genetically inherited.
While his HDL cholesterol was healthy at 1.7 mmol/L, his total cholesterol was 6.94 mmol/L and his LDL cholesterol was 4.3 mmol/L.
Rob says: “I’ve always considered myself pretty healthy. So I was genuinely surprised when I received test results which said I had high cholesterol.
“My doctor mentioned there may be a genetic element to my high cholesterol; something called polygenic hypercholesterolaemia.
“This means I’ve inherited multiple small gene variations that together cause my body to produce or retain more LDL (bad) cholesterol than average.
“Even with a healthy diet and lifestyle, your cholesterol levels may remain high because your liver doesn’t clear LDL cholesterol from the blood as efficiently.”
Dr Guttmann says that around one in 20 people have polygenic hypercholesterolaemia, but it could be less, at one in 100.
Familial hypercholesterolaemia is also inherited and causes extremely high cholesterol from a young age.
According to the British Heart Foundation, you may notice swelling on your knuckles, little lumps in the skin around the bottom of your eye and on your eyelid and/or a pale, white ring around your iris.
“Most healthy adults are advised to have their cholesterol checked at least once every five years,” says Dr Guttmann.
“But if you have a family history of heart disease, you may be advised to start testing earlier (from your 20s or 30s) and to repeat the test every one to three years, depending on your results and other risk factors.”
How to manage and lower your cholesterol
The good news is, once you know you have high cholesterol, you can do something about it.
Rob says: “I eat well, keeping my levels of saturated fat to a minimum, as this is a well-known cause of high cholesterol. I also keep fit and exercise regularly.”
Reducing the amount of fat you eat can help, in particular saturated fat typically found in chocolate, biscuits, cakes, cheese, fatty cuts of meat, pies, palm oil and butter.
The government recommends that men should not eat more than 30g of saturated fat a day and women should not eat more than 20g of saturated fat a day.
For context, an individual pork pie can contain 15g of saturated fat.
Although saturated fats should be limited, healthy fats such as poly and monounsaturated fats should remain in your diet.
Try a 30g portion of nuts and seeds, avocado and/or extra virgin olive oil. Oily fish such as salmon and mackerel are also good sources of healthy fat and protein.
Thought coconut oil was ‘healthy’?
Rob says: “Coconut oil is actually high in saturated fat. It might be fine in small amounts as part of a balanced diet, but there’s no strong evidence that it lowers cholesterol or protects your heart.”
High sources of saturated fat
The NHS warns of these products as high in saturated fat. Check labels of the foods you eat to find others.
Don’t forget about serving sizes. You wouldn’t eat 100g of butter, but that doesn’t mean per serving size, it isn’t rich in saturated fat.
Meanwhile, something like a high-fat beef mince, you are likely to have 125g (500g packet divided by four). That’s more than 10g – half the daily recommended amount – in one food item.
Other things are easy to eat a lot of – like cream and ice cream with dessert.
Fatty cuts of meat
Sainsbury’s British Beef Steak Mince (20% fat): Contains 8.6g of saturated fat per 100g.
Meat products, including sausages and pies
Tesco Finest British Pork Sausages: Contains 9.4g of saturated fat per 100g.
Butter, ghee, and lard
ASDA British Salted Butter: Contains 52g of saturated fat per 100g.
Cheese, especially hard cheese like cheddar
Tesco Mature Cheddar Cheese: Contains 21.6g of saturated fat per 100g.
Cream, soured cream and ice cream
Waitrose Essential Free Range Double Cream: Contains 31.4g of saturated fat per 100ml.
Some savoury snacks, like cheese crackers and some popcorns
ASDA Cheese Twists: Contains 13g of saturated fat per 100g.
Chocolate confectionery
Milkybar White Chocolate Sharing Bar 90g: Contains 18.9g of saturated fat per 100g.
Biscuits, cakes, and pastries
Sainsbury’s Chunky Belgian Chocolate Shortbread: Contains 9.8g per biscuit.
Palm oil, coconut oil and coconut cream
Waitrose Duchy Organic Fairtrade Coconut Oil: Contains 91g of saturated fat per 100g.
Plant power
Swapping some animal proteins for plant-based proteins can also make a difference.
This is especially true if your meat consumption is high in saturated fat – think fatty cuts of red meat (beef, lamb, pork), chicken with the skin on and processed meats (bacon, sausages, salami).
Research in The American Journal of Clinical Nutrition suggests that switching out meat for plant-based meat alternatives for eight weeks or less may help lower total cholesterol by approximately 6 per cent and LDL cholesterol by around 12 per cent.
Rob says: “I switched to soya milk and added more tofu, legumes and tempeh to my meals.”
Sneaky booze
Let’s face it, alcohol isn’t good for much.
Rob adds: “People also tend to ignore the impact of sugar and alcohol, which can contribute to raised triglycerides (a type of fat in blood).”
Triglycerides are a marker of heart health.
“You might have great LDL levels, but if your triglycerides are high, that’s still a risk,” says Rob.
“I’ve cut right back on alcohol, saving it for when I go out. I have a few glasses of wine a week.”
Gut stopper
You also need to add foods that actively help lower cholesterol.
Rob says: “I increased my soluble fibre. This lowers cholesterol by forming a gel in the gut that traps bile acids (made from cholesterol) and carries them out of the body.
“To replace them, the body uses up more cholesterol, which helps reduce LDL cholesterol.
“I now have porridge every morning topped with nuts, seeds, dried fruit and something called psyllium husk, a great source of soluble fibre.”
Other foods filled with soluble fibre include apples, grapes, berries, legumes and vegetables.
A research review in the journal Advances in Nutrition found that taking 10 to 15 g of soluble fiber per day, on average, lead to a decline in LDL cholesterol by about 8 mg/dL.
Past research shows that lowering LDL by 38 mg/dL cuts the risk of major heart problems by about 23 per cent, so this simple addition to your diet could make a significant difference.
If your diet is currently lacking in fibre, increase it steadily over time and drink plenty of water as you do, to avoid bloating and uncomfortable gas.
Carrying excess body fat, especially around the middle, is also linked to higher LDL
Rob Hobson
Rob is also taking Healthspan’s Plant Sterol supplement three times a day.
Plant sterols are naturally occurring compounds that block cholesterol absorption in the gut. They are found in fruit and veg, whole grains, nuts, cheese and milk, but it can be hard to eat enough.
Research in the journal Nutrients showed that intake of 2.4g of plant sterols daily can reduce your cholesterol by up to 10 per cent over two to three weeks.
Rob says: “There’s solid evidence that plant sterols help lower LDL cholesterol naturally when combined with dietary changes.
“Every little helps.”
Increase movement
As well as diet, weight and exercise play a big role in cholesterol.
A review of research in the journal of Heart and Circulatory Physiology shows regular exercise decreases ‘bad’ cholesterol levels in the blood and increases ‘good’ cholesterol levels by stimulating the body to move ‘bad’ cholesterol to your liver, so it can be removed from the body.
Rob says: “I do five gym sessions a week of 30 minutes on the bike followed by 40 minutes of weights.
“I also get in a hot yoga class once a week, and I play badminton a few times a week. I’m always walking everywhere too.
“Carrying excess body fat, especially around the middle, is also linked to higher LDL and triglycerides, and often lower HDL partly because it changes how the body processes and clears fats from the blood.”
But Rob warns that lean people can still have high cholesterol.
Zen and ZZZ
Your sleep and stress can also have an impact on your cholesterol. When layered on top of a poor diet and lifestyle, they make the problem worse.
Rob says: “Chronic stress raises levels of the hormones cortisol and adrenaline, which can change how the liver processes fats, which can nudge up triglycerides and, over time, LDL cholesterol.”
As for sleep, too little can lead to high levels of LDL cholesterol, according to a study published by the Journal of Cardiovascular Nursing.
Individuals in the study who slept less than six hours each night greatly increased their risk of developing cardiovascular disease.
“Poor sleep also alters appetite hormones, making many people crave sugary and fatty foods, which indirectly harms cholesterol further,” adds Rob.
Simple cholesterol-lowering swaps for your daily diet
BREAKFAST
SWAP YOUR…
- High fat croissant for porridge mixed with berries and chia seeds
- Whole full fat milk for semi-skimmed milk
- Fatty bacon and eggs with white buttered toast for scrambled eggs on wholemeal toast with avocado, spinach and tomatoes.
LUNCH
SWAP YOUR…
- Cheese and mayo sandwich on white bread for avocado and tuna on wholegrain toast
- Creamy soups for lentil, chicken or vegetable soups
- Chips on the side for steamed potatoes or a side salad
DINNER
SWAP YOUR…
- White rice for higher-fibre brown rice or quinoa
- Pasta with cheesy, creamy sauce for wholegrain pasta with a tomato sauce and chicken
- Red meat for oily fish, chicken or plant-based proteins
SNACK
SWAP YOUR…
- Crisps for unsalted nuts
- Biscuits for oat cakes with nut butter
- Chocolate bar for two square of dark (70%+) chocolate