When the moment comes for the anaesthetist to place the mask over my little boy’s face, I falter.
While I’ve witnessed my daughter, Vida, go through the same thing on multiple occasions, her medical condition means invasive hospital procedures are necessary to keep her alive, making it easier to fight my protective instinct.
But in two-year-old Gabriel’s case, it is not medically necessary – at least, not for him. The reason my sweet, sparky, wilful boy is in hospital is so he can be a donor for his big sister. My husband and I have chosen this for him – and that knowledge is quietly devastating.
Vida has an ultra-rare genetic blood disorder called Diamond Blackfan Anaemia Syndrome (DBAS). This means she can’t produce enough red blood cells and currently relies on life-saving blood transfusions every three weeks.
Gabriel is being put to sleep so that some of his stem cells can be harvested from the soft centre of his bones, the marrow. By this evening, these stem cells will start being infused into four-year-old Vida in the hope they will take root and kickstart her ability to produce healthy red blood cells of her own.
If it works, this will give her a future that doesn’t tether her to hospitals. The chance of a life in which transfusions, and the medicines that treat their dangerous side-effects, become a thing of the past.
I don’t have anxiety around the procedure itself, having watched Vida go through general anaesthetics and bone marrow biopsies many times before.
But until we got an actual date for it, we downplayed the weight of what Gabriel would endure – the repeated blood tests, the general anaesthetic, the inevitable soreness in his lower back where the stem cells would be drawn and the months of iron supplementation that must follow.
Now, as I gaze at my little boy looking so vulnerable, what we are putting him through is all too real.

Mina Holland with her daughter, Vida, who has an ultra-rare genetic blood disorder called Diamond Blackfan Anaemia Syndrome (DBAS)
This is my son giving a part of himself to my daughter in a way that has the power to completely change the course of her life.
While both my husband Freddie and I would have happily swapped places with Gabriel, he is the one who is a match, not us. My sense of responsibility at our choice – our agency in all this – is dizzying.
But as he drifts into unconsciousness, I still don’t doubt this is absolutely the right thing to do.
Today, stem cells are embedded in the language of our family but, four years ago, I couldn’t have told you what they were – these building blocks of blood and of life, tiny but potent, capable of becoming red cells, white cells, platelets.
Freddie, a musician and sound designer for TV and film, and I, a journalist, met Bridget Jones-style in my aunt’s kitchen between Christmas and New Year 2013, our parents having friends in common.
We planned a family together from the start; Vida came along almost two years into our marriage.
The pregnancy was smooth until the end, when scans started to show high readings that suggested my placenta might be failing (in hindsight, we suspect this may have been linked to her condition, although we will never know for sure). She was delivered by caesarean at 37 weeks.
Vida was 11 weeks old when we first discovered, at what was meant to be a routine hospital follow-up, that something was seriously wrong.
It was supposed to be a box-ticking appointment, the kind that disappears into the fog of early parenthood.
But the moment the doctor saw her and registered the startling pallor of her skin, she was admitted immediately for an emergency blood transfusion.
When the doctor asked me: ‘Did you not see?’ I felt the wall, the ceiling, faces and furniture begin to melt.
Because the truth is, yes, I had seen something – I just hadn’t known what.
I had noticed how other babies were feeding better, sleeping for longer and settling into routines, while Vida wasn’t.
I’d noticed how pale she looked during bath times, especially when I compared her skin to mine.

I had noticed how other babies were feeding better, sleeping for longer and settling into routines, while Vida wasn’t, writes Mina
But as a first-time parent I assumed it was just the contrast between a baby’s soft complexion and an adult’s skin. I didn’t realise it was a sign of severe anaemia.
And, in any case, each time I did voice a worry about her development, my mother’s intuition was met with smiles, reassurance and kindly dismissals.
The GP, the midwife, the lactation consultant – they’d all told me she was fine and, of course, I wanted to believe them.
My concern got absorbed into the narrative of new motherhood; brushed aside as exhaustion, anxiety, hormones. When the DBAS diagnosis came seven weeks later, we learned that without transfusions every three weeks, she wouldn’t survive.
Gone was the parental routine I’d imagined, of baby groups and meeting up for coffees and moaning about the trials and tribulations of new motherhood with other sleep-deprived mums.
Immediately, every part of my life rearranged itself around the stark reality of Vida’s condition, observing how she perked up with fresh blood and declined as she ran low again.
Mornings dissolved into transfusion schedules, while afternoons got swallowed up with research as the journalist in me tried to better understand her condition.
It was a problem that I, as her mother, felt was my duty to fix. The nights were swallowed by anxiety over treatment side-effects and test results.
I swung between an obsessive search for hope and feeling utterly hopeless. I fretted over blood counts, second-guessing every symptom, every therapy, every doctor’s opinion.
It felt as if the only way to stay afloat was to dive headfirst into knowledge and options, even at the cost of my own mental health.
While I scrolled through my phone, looking for answers, Freddie went to work.
He also cooked, swooped Vida off for early-morning walks and researched all the stuff I didn’t seem to get to – bottle brands, nappy bins, age-appropriate bath toys, even baby sunglasses.
Some days I envied his ability to suspend the same heavy feelings that weighed me down.
But my way of giving myself some semblance of control was to become as informed as it was possible for anyone to be, even if I felt other people’s fatigue around my obsession, because DBAS became all I talked about.
I learnt about the imperfect treatments for it; the significant complications that come with a lifetime of transfusions – namely the build-up of iron in the body’s organs, which can be dangerous.
And how Vida’s bone marrow might eventually be shocked into producing those precious red cells by high-dose steroids, but at the cost of physical growth, bone density and her immune system.
Mina’s book details what it was like caring for a baby with such a rare illness
The most definitive treatment for Vida would be a bone marrow transplant. But it was risky; her entire immune system would need to be destroyed in the process. It would mean a year out of mainstream life. But if successful it would liberate her from transfusions and their side-effects.
I wanted the closest thing to a fix and so, despite its risks, I was drawn to the idea of this. But for a patient or their parents to have that choice, they need either to have a matched sibling donor – the gold standard of donors for their superior genetic similarity to the patient – or to have exhausted all other treatment options, which would qualify them for a transplant using an unrelated donor from the bone marrow register.
I knew which option I preferred. Freddie and I wanted another child anyway and so we started to look into having another baby via IVF, using a process called pre-implantation genetic testing that would enable us to engineer a donor for Vida – otherwise, siblings only have a 25 per cent chance of being a match.
At first, Freddie was reluctant to think about another baby while I seemed so focused on fixing’ things.
But he also recognised how this ‘project’ (for want of a better word) was helping me to feel I wasn’t impotent in all this.
And so began what some might call ‘playing God’.
First, we had to get approval from the Human Fertilisation and Embryology Authority (HFEA), because any embryos created would be genetically screened in order to produce a baby who would be Vida’s genetic match.
I was aware of the controversy surrounding embryo selection, but we weren’t choosing a baby based on eye or hair colour or sex, indulging an aesthetic preference or a predilection for appearance or personality.
Our child would be a much-wanted family member who happened to have a trait that could help their sister in a way no one else could.
We were choosing traits invisible to the eye: stem cell compatibility that could give our daughter a better life. We wanted to give Vida the best chance we could.
Who could possibly argue with that? Plenty of people, it turned out, but I limited my exposure to them, keeping my echo chamber small and validating.
If terms like ‘designer baby’ take a swipe at the parents, ‘saviour sibling’ loads responsibility on to the child that results from this kind of IVF.
A matched sibling could change Vida’s life, but it wouldn’t be their duty to do so – if they chose not to, or if it didn’t work, there would be no failure on their part.
Even with a perfectly matched sibling donor, bone marrow transplants are complex medical procedures, not divine interventions. But the medicine could help, so we were calling on it.
In the end though, soon after the HFEA licence came through, we had to give up on the idea of IVF.
My body failed to respond to the medication meant to stimulate it into producing the extra eggs needed for this treatment. It was game over.
This now meant that if Vida ever needed a transplant, we’d have to put our faith in an unrelated donor. Unless we conceived a matched sibling baby naturally.
Thankfully, Gabriel was conceived quickly and when he was born in December 2020, we chose that name because an angel was exactly what we needed.
If there is a God then he played his part, because at two months old tests revealed he was a genetic match for Vida.

Mina, her husband Freddie with Vida and Gabriel – who, after the couple had to give up on IVF, was concieved naturally and was thankfully a genetic match for his sister
But there was also no escaping how our children’s early lives would now be shaped by the choices Freddie and I made.
When your child faces life-threatening illness, the stakes skyrocket. Things such as deciding when to go back to work or picking the best school seem insignificant.
I found myself asking questions no parent ever expects: should we risk a transplant for Vida? Should Gabriel give a part of himself, albeit a part he could replenish in time, for a chance at good health for his sister?
The responsibility to get it right felt colossal, keeping us both awake at night.
In the end, knowing that we had our perfectly matched boy, along with emerging research about improved quality of life outcomes for post-bone marrow transplant patients with blood disorders, we were nudged in that direction.
From the start, there were systems in place to protect Gabriel, who had to be at least two to donate.
He has his own consultant to assess his fitness for donation and to represent his interests.
During our counselling sessions with the hospital, required before this kind of procedure, Freddie and I were asked ‘what are the benefits to Gabriel?’
Our response: to have a sister who is in the best possible health for the longest possible time.
Donating bone marrow sounds invasive – it is, after all, the extraction of part of someone’s precious blood factory (in this case, from the core of their hip bone). But it’s also virtually the same process that Vida herself had been through during many biopsies, so it felt familiar.
For Gabriel, it meant a general anaesthetic and anaemia we’d treat with iron supplements. Weighed up against having a chronically, increasingly unwell sister, it seemed reasonable to proceed.
Still, it meant putting Gabriel through experiences he didn’t enjoy. He was incensed that anyone might try to restrain him while brandishing a stethoscope or, worse, a needle.
And while Vida would bounce back fast from the likes of a blood test, Gabes’ mood stayed bruised by the interventions of a doctor or nurse. He would tell me that he didn’t like ‘dat red night’ (the oxygen saturation monitor), or ‘dat sharp fing’ (a needle).
Gabriel donated his marrow in the early morning of March 8, 2023. Vida had already endured a week of chemotherapy to wipe out her immune system and so – later that same day – her transplant began.
This wasn’t a quick fix. There were 15 months of hospital stays, splitting us as a family and meaning bedtime stories got told over FaceTime for one of our children each evening.
We had to sanitise everything – even boiling her drinking water – and shun mainstream life in order to protect Vida from the risk of an infection she didn’t yet have the immune system to fight off.

While the transplant seemed equal to the medical processes Vida had gone through, it still meant putting Gabriel through things he didn’t enjoy. Today both children are thriving and have a strong bond
I took a period of indefinite leave from my job to become a full-time caregiver, while our world as a family shrank.
But the transplant marked a very real turning point. Vida’s immunity began rebuilding. Our freedoms returned slowly – playgrounds, nursery, work, piece by piece.
And as a mother, I relearned how to stay present.
The fear didn’t vanish – Vida will always need to be closely monitored – but those months of chaos, of love and terror, shaped me. I’m a better, kinder, more patient person as a result.
Today, the children are four and six and both are thriving.
Vida started school midway through her reception year and is doing well, despite still having many hospital appointments. Gabriel will join her in September.
But their fiery squabbles notwithstanding, we see the strong bond between our kids.
How, if Vida is given a snack or a toy, she’ll always ask if there’s one for her brother. The way that, when we pick him up from nursery, the first thing Gabriel asks is: ‘Where’s Vida?’
Watching them in scenarios so many parents take for granted –playgrounds, swimming pools, even just drinking tap water – I am reminded these things weren’t always possible; I will never stop feeling grateful that they now are.
We believe Gabriel would have chosen to do this for Vida if he could, and that one day he will be proud to know what he did.
It was the hardest decision we ever had to make. But we feel clear about the pay-off – for both our children.
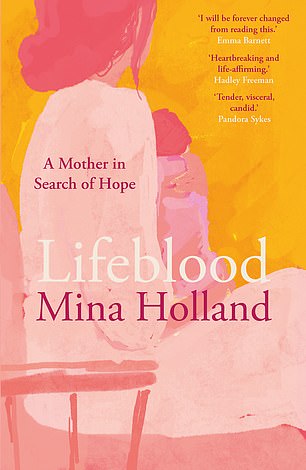
Adapted from Lifeblood by Mina Holland (Daunt Books, £10.99) out now. © Mina Holland 2025. To order a copy for £9.89 (offer valid to 12/07/25; UK P&P free on orders over £25) go to mailshop.co.uk/books or call 020 3176 2937.












